 At the November 2019 Quarterly meeting of the California Medical Board of California as agenda item (11-B) was formally proposing that the Board carry a bill that would make it illegal for Ca LMs to provide care VBAC care.
At the November 2019 Quarterly meeting of the California Medical Board of California as agenda item (11-B) was formally proposing that the Board carry a bill that would make it illegal for Ca LMs to provide care VBAC care.
This made me so angry I wanted to cry, as we already spent nearly 4 years (2002 to 2006) fighting with the Md Bd’s staff, CAM, ACOG, and representatives of CAM, CCM and C-Fam.
It was only through Divine Interventions (the only possible explanation given the massive resources stacked against us) that we finally worked out a mutually satisfaction “VBAC Compromise” in 2005 with the help of Dr. Richard Fantozzi (Board president), two ACOG representatives, and Md Bd members on the Midwifery Task Force in addition to CAM & CCM.
It breaks my heart to be have all the stripped out from under us by AB 1308 and now to have ACOG working aggressively to drag midwifery back into another fighting war over VBAC.

OB patient being ‘prepped’ for Cesarean surgery
So I am reposting this as history of the war we already fought and won and now it seems we are going to have to start all over again.
faith gibson, LM ^O^
DRAFT Version
(so far not able to locate the final version)
California College of Midwives
Palo Alto, CA 94303
650 / 328-8491
Medical Board of California
1426 Howe Avenue
Sacramento, CA
July 29th 2005
Testimony: Continuation of Regulatory Hearing July 29th, 2005 // Oppose Midwifery Standard of Care Regulation as Currently Proposed
The consensus belief of the California College of Midwives et al, is that the original regulatory proposal (July 2002) not only fulfills the legislative mandate of SB 1950, but is the superior choice.
That language read:
(b) The standard of care shall be that of the California community of licensed midwives.
Authority cited: Section 2018 and 2507(f) Business and Professions Code Reference: Section 2507.”
 Editor’s Note — there are a few places in this draft that are still unfinished, but so far i haven’t been able to find the final draft submitted to the MBC.
Editor’s Note — there are a few places in this draft that are still unfinished, but so far i haven’t been able to find the final draft submitted to the MBC.
Overview & Legislative History
SB1950 directed the MBC “to adopt regulations defining … the appropriate standard of care for the practice of (licensed) midwifery”. According to conversations with Senator Figueroa, the bill’s author, before and after the passage of SB 1950, accompanied by letters from her to the MBC (copy enclosed) the legislative intent for this statute was to establish that the appropriate criteria for California licensed midwives was a midwifery-based standard and not an obstetrical standard.
This has become an issue because the MBC staff referred quality of care issues to obstetricians for expert review. The results are consistently negative assessments of the licensed midwife’s care, which were then became the foundation for disciplinary actions against the LM. However, obstetricians are not educated, trained or experienced in the discipline of midwifery, especially as provided in a community-based setting, and therefore do not have the knowledge base to define the appropriate ‘standard of care’ for licensed midwives.
The consensus of scientific research on maternal-infant outcome statistics for community-based midwifery care as currently practiced by California LMs is equal in perinatal mortality to those of hospital-based obstetrics.
However, midwifery care resulted in a three to five-fold reduction in medical interventions and Cesarean sections, thus it cannot be claimed that obstetrical review is more appropriate or more ‘expert’ for the non-medical discipline of midwifery . [copy enclosed of BMJ 6/18/05 research on CPM-attended home birth]

California Senator Liz Figueroa, author SB 1479 (2000), SB 1950 (2002) & SB 1638 (2006)
Midwives are experts in midwifery and obstetricians are not. SB 1950 (2002, Senator Liz Figueroa) was a legislative remedy mandating that an appropriate midwifery standard should be identified in regulation and that midwifery standards, in conjunction with expert review by licensed midwives (but not obstetricians), should be referenced whenever the Board was contemplating or pursuing disciplinary action against a midwife licentiate.
The legislative authority for the standard of care regulation (SB 1950) does not refer to, or authorize any change in the licensed midwife’s scope of practice. In fact, the words “scope of practice” do not appear anywhere in the language of SB 1950. Any desire by the American College of Obstetricians and Gynecologists (ACOG) to re-define the scope of practice under the LMPA of 1993 should be addressed to the Legislature. Restrictions to the licensed midwife’s scope of practice cannot lawfully be incorporated via the backdoor, through an unauthorized rewriting of the midwifery standard of care by ACOG as subsequently proposed by the MBC.

California Senator Lucy Killea, author of Licensed Midwifery Practice Act of 1993 (SB 350)
According to the original language of the LMPA of 1993 and the 2000 amendment (SB 1479, 2000, by Senator Figueroa), midwifery is a distinctly defined profession separate from both the practice of medicine and the practice of nursing. Distinct qualities of community-based midwifery practice are most clearly identified in the intent language of SB 1479, Sec. 4, particularly subsection “c”:
~ SB 1479 (2000) THE LEGISLATURE FINDS AND DECLARES THAT:
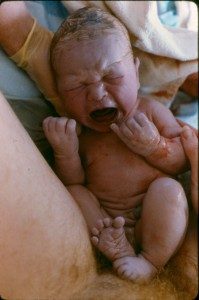
(a) Childbirth is a normal process of the human body and not a disease.
(b) Every woman has a right to choose her birth setting from the full range of safe options available in her community.
(c) The midwifery model of care emphasizes a commitment to
-
- informed choice
- continuity of individualized care
- sensitivity to the emotional and spiritual aspects of childbearing
and
-
- includes monitoring the physical, psychological, and social well-being of the mother throughout the childbearing cycle
- providing the mother with individualized education, counseling, prenatal care, continuous hands-on assistance during labor and delivery, and postpartum support
- minimizing technological interventions
- identifying and referring women who require obstetrical attention
(d) Numerous studies have associated professional midwifery care with safety, good outcomes, and cost-effectiveness in the United States and in other countries. California studies suggest that low-risk women who choose a natural childbirth approach in an out-of-hospital setting will experience as low a perinatal mortality as low-risk women who choose a hospital birth under management of an obstetrician, including unfavorable results for transfer from the home to the hospital.
(e) The midwifery model of care is an important option within comprehensive health care for women and their families and should be a choice made available to all women who are appropriate for and interested in home birth.
 Adoption of a Midwifery Standard of Care that is consent with its authorizing legislation (SB 1950) and the the Licensed Midwifery Practice Act of 1993
Adoption of a Midwifery Standard of Care that is consent with its authorizing legislation (SB 1950) and the the Licensed Midwifery Practice Act of 1993
It is the understanding of the midwifery community, specifically confirmed by Senator Figueroa’s office, that the Medical Board has only been mandated by SB 1950 to “adopt” (but not to draft) the standard defining the appropriate practice of midwifery. A formally documented (i.e., written) midwifery standard of care describes a retrospective process that records ‘standardized’ care as it is currently provided by licensed midwives. This definition would be in conjunction with scientific definitions of technically competent, ‘state of the art’ care.
 Defining the appropriate practice of community-based midwifery, in light of the legislative language and intent of the LMPA and its two amendments (SB 1479 and SB 1950), would be a process entered into by those educated in, licensed in and experienced in the practice of midwifery in the state of California.
Defining the appropriate practice of community-based midwifery, in light of the legislative language and intent of the LMPA and its two amendments (SB 1479 and SB 1950), would be a process entered into by those educated in, licensed in and experienced in the practice of midwifery in the state of California.
This process also takes into account that ‘standard practices’ would be consistent with science-based definitions of competent care, as can be identified from textbooks, other educational sources, scientific research as reported in peer-review journals and the testimony of ‘customary practices’ by practicing midwives.
California College of Midwives’ Conclusion and Recommendations
It is the official position of the membership of the California College of Midwives (CCM) that the specific language of the CCM Standard of Care (sections 1 & 2 — copyrighted Oct 2004) as originally “referenced” in the MBC proposed regulation (Nov 2004 and February 2005) and the general language of the MANA standards would both fulfill the intention and legal necessities of SB 1950.
However, we believe that the original (July 2002) regulatory proposal not only fulfills the legislative mandate of SB 1950, but is the superior choice.
That language reads:
(b) The standard of care shall be that of the California community of licensed midwives.
Authority cited: Section 2018 and 2507 (f) Business and Professions Code Reference: Section 2507.”
Furthermore California licensed midwives, uniformly and totally, reject ACOG’s unauthorized re-writing of the California Collage of Midwives Standard of Care. At the most basic level, it is copyright violation., this unauthorized version is falsely claimed to be a mere ‘modification’ of the former language proposed at the November 2004 and February 2005 regulatory hearing.
In addition, we strenuously object to this regulatory hearing being characterized as a “continuation” of the previous hearings. The changes proposed are not merely ‘substantive’ but in fact are massive and a complete break with all that has gone before.
Therefore, we believe that it is inappropriate for the OAL to proceed with any further review of this regulation as proposed.
In addition, we also believe that the ACOG authored so-called midwifery standard fails on all the formal parameters for regulatory conformation as noted below:
Lack of Authority: The appropriate standard of care for the practice of licensed midwifery would be a midwifery standard as designated by the California community of midwives. Therefore we believe that the MBC is not authorized to draft language separate from the California community of midwives.
Necessity:
Duplication:
Etc, etc, etc………..Unfinished
The Purpose and Goal of the LMPA
The purpose and goal of the LMPA was to make professional maternity services legally available to essentially healthy childbearing women who, for personal, philosophical, cultural, economic or religious reasons, have chosen non-obstetrical pregnancy and childbirth care.
Explicit and implicit in the licensing statue and its amendments is the acknowledgment that the safety of out-of-hospital midwifery care for healthy women with normal pregnancies, which is to take place in conjunction with access to appropriate obstetrical services for complications. {1} This form of midwifery care is statistically equal to hospital-based obstetrical care for the low and moderate risk population, while unattended childbirth {2}, especially in women with no prenatal care of orders-of-magnitude risker than either obstetrician or midwife-attended birth.
{1} Alternative in Childbirth, Peter Schlenzka, 1999;
{2} Study #1 Perinatal & maternal mortality in a religious group avoiding obstetric care – Am Jour Obst Gyne 1984 Dec 1: 150(7):926-31:
(Note: Out of 344 births, the unattended birth group 6 maternal deaths and 21 perinatal losses. The baseline mortality rate for unattended childbirth was one maternal death per 57 mothers or MMR of 872 per 100,000 live births (92 times higher than Indiana’s MMR for the same period) and one perinatal death for every 16 births or PNM rate of approximately 45 per 1,000. {see addition note at the end of this document for further details}
When the statistical model is extended to include the downstream adverse events and complications generated by the high rate of cesarean delivery associated with the medical model (approximately 27%), the physiological management is identified as significantly safer for healthy women than the medicalization of normal childbirth in an essentially healthy childbirth population (70-85% of all childbearing women).
However perinatal mortality statistics for unattended birth (which for many women is the only acceptable or available alternative to obstetrical care) has been shown by researcher to be up to 30 times higher than the care of even lay (i.e., non-professional) midwives (3 out of a 1,000 vs. 60 to 120).
In the last few years, as women with a certain pregnancy status are increasingly refused non-surgical obstetrical care (i.e., only care offered by obstetricians was Cesarean delivery), a grass-roots movement promoting unattended childbirth has arisen. Members of this movement refer to themselves as “UCers” for “Unattended Childbirth” In more recent years a number of Internet web sites have been developed that circulate ‘how-to’ instructions and streaming video of unattended births. However, it is clear from statistical resources, as well as the common experience of professional midwives, that mothers and babies are always safer with a professional in attendance than they would be without such a safety net.
While it runs counter to the way most American think of the subject and may even offend some members of the medical profession, professional midwife-attended birth in any setting is safer for healthy women than either obstetrical intervention or unattended birth. This fact is consistent with the background and legislative intent of the 1993 LMPA, whose purpose was to reduce the number of women who were unable to find appropriate care and thus might instead choose unattended childbirth.
Standards and Guidelines vs. Scope of Practice
Midwifery standards and guidelines provide protective guidance to the practitioner by delineating minimum expectations. The goal of this official information is to provide safe, “state of the art” care to consumers, protect individual clients from substandard care and protect the practitioner from litigation and accusation of unprofessional conduct that may arise out of a lack of consensus from within the profession.
Standards of practice are not the same as a scope of practice, nor are standards interchangeable with “scope of practice”. The scope of practice for licensed midwives is fixed by statute, which authorizes licensed midwives to provide care for normal childbirth, prohibits the use of “artificial, forcible or mechanical means” and requires that significant complications be immediately referred to a physician.
SB 1950 mandate to the MBC does not authorized any re-definition of the scope of practice for California LMs.
The LMPA states that the license to practice midwife does not authorize the holder to practice medicine or surgery. In addition to this provision in the LMPA, other sections of Chapter five of the B&P code also define the unauthorized practice of medicine as any unauthorized use of drugs and surgical instruments. These limitations and prohibitions would prohibit podalic version (internally turning a head down baby into a breech and then extracting the baby by the feet). It also prohibits the use of pharmaceutical drugs to induce or accelerate labor and/or the use of forceps or vacuum extraction to facilitate delivery.
The Licensed Midwives Practice Act of 1993 specifically authorizes the LM to attend cases of ‘normal birth’. While it does not describe or otherwise define ‘normal birth’, the LMPA does define the obverse — abnormal birth would be parturition (i.e. intrapartum period of labor and birth) in which there is a need to use “artificial, forcible or mechanical means“.
This specific language tracks back to the midwifery licensing law passed by the municipality of Rochester, New York, in 1896. This language defining prohibited activities was then used in the 1917 non-nurse midwifery provision of the California Medical Practices Act, the 1974 California nurse-midwifery licensing act and most recently in the 1993 LMPA.
The message from physicians (who were the framers of these statutes) was clear and broke down along classic gender lines — boy-toys versus girl-toys. The girl-midwives got spontaneous, ‘nothing-to-do-but-stand-by-and-watch-the-baby-come-out’ normal, non-medical childbirth and the boy-doctors got to use the fun toys – drugs and forceps. The 1917 midwifery certification provision of the MPA clearly states in its introductory paragraph that the purpose of midwifery provision is to provide penalties for midwives who stray into the “boy-toy” category by using drugs or instruments.
The classical definition of ‘normal’ recognizes that normal equates with normal spontaneous biology (i.e., not artificially stimulated) that is not pathological in its progress or its effect. It refers to spontaneous physiological processes that are characteristic of healthy reproductive biology of childbearing women and can reasonably be expected to lead to normal or spontaneous conclusions.
Functional Definition of Normal and the Issue of Perceived Risk
Normal is also associated with a state of irreducible risk that is, all other responses add, rather than subtract, risk.
Normal childbirth may be distilled into the following definition (CCM Standard of Care:
“Normal as used by the LMPA would refer to a pregnancy that naturally advances to term with a live, growth-appropriate fetus/fetuses in a vertical lie, and culminating with a spontaneous labor that can reasonably be expected to lead to a spontaneous live birth of a viable neonate, with conservation of the health and wellbeing of both mother and baby.”
{{ Editor’s Note: Dr Pat Chase, an MD consultant assigned by the MBC in 2004-2005 to compile a midwifery standard of care (per SB 1950) for the Medical Board remarked in a letter that the ” …. definition of “normal birth” in the California College of Midwives 2004 Standard of Care and Practice Guidelines was the most complete and easy-to-understand definition of normal birth that she’d ever encountered”. }}
This simple definition of “normal birth” is generally accepted by midwives around the world is applied to a healthy mother who is pregnant with a fetus/fetuses in a longitudinal lie (either vertex or breech) with spontaneous onset of labor after 37 weeks of pregnancy and progresses in a timely manner through out the various stages and phases associated with physiological parturition while the mother and baby are able to remain adequately hydrated and free of pathological distress.
Risk vs. Complication: The Licensed Midwifery Practice Act of 1993 prohibits providing care to childbearing women with a medical complication. However, the LMPA is silent about the topic of risk, which is a mathematical equation for the future possibility of a complication.
Risk is an elevated possibility that a specific accident, illness or complication will occur. It is not a probability — merely a possibility — and that possibility is usually a small fraction expressed as ‘one out of a hundred’ or whatever is accurate for the particular topic.
This example would mean that for every one person that had the complication, 99 would not have any negative consequence. For instance, a history of heart disease in the family or a high cholesterol level is not the same as having a heart attack. Most people with either of those conditions never have a heart attack. Few people would be willing to have a surgical procedure done on their heart ‘prophylactically’, since the actual performance of surgery exposes one to the high level of immediate risk for surgical complications, as well as pain, expense and the possibility of having long-term disability or the need for additional surgeries to correct problems resulting from the initial surgery.
ACOG’s Proposal to Redefine the Midwife’s ‘Scope of Practice’
ACOG’s proposal for a midwifery standard of care advances the notion that a small specific list of risks, ones proposed by them, would henceforth constitute “abnormal” cases of childbirth.
They suggest in their letter to the MBC that should the Board define these situations as outside the scope of practice for LMs via the currently pending regulation, any midwife who subsequently provided care to women with these pregnancy circumstances would be considered guilty of an ‘illegal practice of medicine’. We refute this assertion based on three principles.
First Point: The plain reading of the LMPA does not support this idea. An uncomplicated pregnancy and spontaneously progressing normal labor with no identified, present-tense complication would be ‘normal’ in the meaning of the LMPA, with its high propensity to conclude with a normal birth, absent any intervening complication, in which case the requirement to refer to a physician would supersede.
For example, a 1999 ruling by the Office of Administrative Hearings judge in the Alison Osborn case in confirmed that a licensed midwife may provide care to a mother with a breech baby who has declined Cesarean delivery and withdrawn from obstetrical care, as long as the midwife obtains appropriate informed consent/informed refusal and the LM has appropriate additional training and specific protocols relative to the circumstances (copy OAL ruling enclosed).
Another document demonstrating this is a letter from a MBC investigator dated Jan 2004 to an LM regarding an investigated conducted by the Medical Board into her care of a planned home birth client who transferred to the hospital during labor. According to the text of the letter:
“the expert who reviewed the case concluded that there was no departure from the midwifery standard or care in regard to your handling of Ms. ——-‘s VBAC.”
“The investigation related to [client name]. has been closed. We would like to thank you for your cooperation with the investigation.” (copy MBC letter attached).
Second point: Any desire by organized medicine to modify the scope of practice for midwives would require a legislative remedy, which would provide for legislative hearings, testimony and letters and other forms of public participation, so as to guard against any self-serving limitation being put on midwifery practice by ACOG that were not consistent with the best interest of the public.
Third Point: It is not appropriate for either ACOG or the MBC to redefine the ‘illegal’ practice of medicine in regard to midwifery, as the MPA and the LMPA both provide a black-letter definitions. That definition does not extend to, or incorporate, the category of mere mathematical ‘risk’, but instead requires a specific action relative to unauthorized medical or surgical activities or critical omissions.
Section 2052 of the MPA prohibits unlicensed persons from diagnosing, treating, operating upon or prescribing drugs, prohibits the use of ionizing radiation and the severing or penetrating human tissue (beyond the severing of the umbilical cord).
The LMPA prohibits the furthering of childbirth by any “artificial, forcible or mechanical means” and it also notes an obligation to refer complications “immediately” to a physician, which means that the law prohibiting the unauthorized practice of medicine can be violated by omission (failure to refer) as well as commission (use of drugs and surgical instruments).
Neither legislative act mentions a scheme for parsing relative risks into specific categories and then requiring additional actions based on such categories.
ACOG asserts that neither the mother nor the midwife may “waive” what they define as the ‘restrictions’ of the LMPA against the unauthorized practice of medicine. The example they use is the notion that a chiropractor could not, under the theory of informed consent or informed ‘refusal’, perform a Cesarean section at the request of a patient.
We absolutely agree that performance of a CS would indeed be an illegal practice of medicine.
However we also absolutely disagree providing normal non-medical childbirth services to a healthy woman with a normal pregnancy who has an identified risk factor (and fully informed patient consent) would be defined as an illegal practice of medicine. This is premised on the notion that a childbearing woman with a risk factor has no right to refuse unwanted prophylactic medical intervention and thus qualifying the care provided by a Ca LM as an illegal practice of medicine.
Midwives performing surgery is obviously illegal (and had nothing to do with implementation of SB 1950), while midwifery providing normal midwifery care to an essentially healthy consenting adult woman with no signs or symptoms of a current complication is NOT equivalent to illegally performing surgery or illegally practicing medicine.
For healthy women, medical and surgical interventions increase the complication rate. In the US, deaths from iatrogenic causes is one of the top five causes of fatality, exceeding the annual deaths from breast cancer, all house fires and all plane crashes.
Once the mother-to-be has declined obstetrical treatment, nothing in the LMPA prevents the LM from providing physiological midwifery care to this mother, as physiological care is, by its very nature, non-medical and thus it is not an “illegal” practice of medicine (unlike the earlier example of performing a CS). Physiological care is a safety net (the mother’s ‘shield) which should not be interpreted as a ‘medical procedure’, thus turning it into a sword.
VBAC, breech, and twin pregnancies all have an identified risk factors associated with them, but none of these situations requires the administration of drugs or medical procedures to preserve the health of either mother or baby. These states do not require any medical treatments to initiate progressive labor, nor is surgical delivery mechanically necessary, unless a specific complication actually occurs.
In most parts of the world, healthy women with these pregnancies, who receive appropriate prenatal care, have their labors physiologically managed and have spontaneous vaginal births, with outcomes for both mom and baby equal to those of a first pregnancy. A several large recent studies of the VBAC risk to the neonate show that planning a natural labor in post cesarean mothers to results in the same neonatal mortality as first-time mothers, while the “risk-reduction” choice of Cesarean actually add the above list of 15 additional complications without improving outcomes for the baby.
The big issue in the United States is that physiological management is not an option offered by the obstetrical profession. In America, obstetricians routinely perform cesarean surgery in all of these cases, a situation brought about by liability concerns and physician preference. By its own reports, the science of obstetrics was not designed nor structured to promote normal birth or reduce the incidence of medicated labors or surgical interventions in normal births. It was and is organized around detecting and treating the rare complications, which makes its practitioners, who are trained as surgeons, ill-suited to provide routine care to health women, a fact attested to by a 27% Cesarean section rate.
The numbers of Cesareans needed to be performed to prevent a single adverse event (i.e., NNT or ‘numbers needed to treat’) for the above situations is in the hundreds (ObGynNews stats is 1:500. This meaning the other 499 Cesareans had no benefit to either mother or baby, but did expose the childbearing women to iatrogenic complications during the current birth and exposed both mother and baby to post-cesarean complications in future pregnancies. Given the long list of dramatically increased dangers associated with surgical delivery, not to mention pain and disability of surgical delivery, a healthy, mentally-competent woman has the constitutional right to decline obstetrical treatments that are not wanted, medically necessary and which increase the likelihood of serious complications.
Nothing in the plain reading of the LMPA would lead anyone to assume that an ‘informed refusal’ by a mentally competent woman of unwanted medical intervention would prevent her from seeking out the physiologically-based care of a professional midwife or prevent the midwife from providing such care as it was consistent with the parameters of the LMPA – no artificial, forcible or mechanical means, while any complications would be referred immediately referred to a physician. I have also provided a list of the 51 (out of 55) certified nurse and licensed midwives from three states (California, New Mexico and Florida) who had malpractice coverage with a professional liability consortium who stated, in their application to join the group policy, that they routinely attended VBAC labors in out-of-hospital settings.
Also included in the enclosures is a document produced in Australia that tracks the irreducible or “native” risks of childbearing and compares those numbers to mortality or morbidity associated with normal labor and vaginal birth, Cesarean delivery, VBAC and Cesarean risks that accrues during subsequent pregnancies, labors and VBAC.
Its conclusion is that:
“The likelihood of a fatal outcome from a uterine rupture is no higher than the general incidence of death in all births and is lower than that for Cesarean birth.”
When is a Risk a RISK?
While the 3 categories listed by ACOG – VBAC, breech and twin pregnancies — are ‘dramatic’ and easy to understand examples of risk, the real issue is the right of childbearing families with normal pregnancies to decline unwanted medical care when there is any possibility of an adverse event, which is basically most of the time.
For example, Christian Scientist patients legally (and consistently) decline all prenatal lab work, genetic testing and ultrasound examinations. This exposes them and their unborn or newborn babies to the risks associated with undiagnosed anemia, a high white cell count, low platelet levels, an RH negative baby with a positive titer, a misdated pregnancy or one with potentially-fatal congenital anomalies or that is a breech or twin pregnancy.
Other women refuse diabetic screening (risking a big baby with shoulder dystocia), some families live unusually far from a hospital or up in the hills in hard to reach places or go into labor during a snow storm. Many women refuse group-B testing or after testing positive for GBS refuse prophylactic antibiotics. Most clients of midwives decline sequential ultrasounds in the last trimester, risking the possibility of undiagnosed twins, breech or big baby.
Some women have their water break before active labor, have a slow (but not abnormal) labors or are carrying a bigger than average baby who is at added risk for shoulder dystocia and excessive maternal bleeding after delivery. All these risks can result in a perinatal death or disability, at rates approximately the same as the VBAC risk. What is the qualitative legal difference between the risks associated with VBAC, breech and twin pregnancies, which ACOG would like to have designated as an illegal practice of medicine, and all the other garden-variety types of ‘moderate’ risks that follow the informed refusal of medicalization by healthy, mentally competent childbearing women?
ACOG’s own policy manual [ ACOG Compendium, p. 160; No 214, April 1999], acknowledges the principles of body integrity for women in regard to reproductive biology. In a position statement on conflicts in the maternal-fetal relationship and patient choice, it states that
“Medicine aims to foster the greatest benefit with the least risk. Risks and benefits however may be valued differently by pregnant women and the obstetrician…”
In interactions with a woman who appears to resist following medical advise, it counsels that
“ the obstetrician must keep in mind that medical knowledge has limitations and medical judgment is fallible. … Existing methods for the detection of non-reassuring fetal status are not always reliable indicators of poor outcomes and there is often insufficient evidence for risk determination or risk-benefit evaluation for the fetus.”
It goes on to say:
“the obstetrician must respect the patient’s autonomy, continue to care for the pregnant woman, and not intervene against the patient’s wishes, regardless of the consequences.”
In general ACOG already acknowledges the right of mentally competent women, under the theory of informed refusal, to refuse medical treatments even when the decline of these interventions is perceived by medical authorities to disadvantage the fetus. According to an appellate court decision in an ACOG case, the bar for over-riding the autonomy of the mentally competent women via court-ordered intervention is to be reserved for “extremely rare and truly unusual circumstances”.
The ethical principle here, which is predicated on both the autonomy of the childbearing unit and the fallibility of medical science and its historically paternalistic relationship to the topic, it that risk reduction must always be implemented with the consent of the parents. Otherwise we open the door for special interest groups to force all manner of competent adults into prophylactic medical treatment and drug regimes based on someone else’s idea of “what is good for us”.
(Note: The above language of “extremely rare and truly unusual” was taken from an appellate court decision (DC Appeals Court 1991-quoted Gabbe’s Obstetrics, Ch 42 – legal issues) in an ACOG case that confirmed the right of mentally competent women to decline unwanted medical or surgical interventions even if there is concern about the well-being of the fetus).
{ 0 comments }
Public Comment ~ Virtual Medical Board Meeting, May 7th 2020
 My name is Faith Gibson. I’m a Cal licensed midwife and was a member of the Midwifery Advisory Council from 2007 to 2013.
My name is Faith Gibson. I’m a Cal licensed midwife and was a member of the Midwifery Advisory Council from 2007 to 2013.
I’m requesting support by the Medical Board for an amendment to the Licensed Midwifery Practice Act of 1993 to expand the postpartum scope of practice of licensed midwives from 6 weeks to 12 months. This is consistent with definitions used by the CDC and World Health Organization for assessing maternal health and tracking maternal morbidity and mortality.
We generally think of maternal deaths as primarily a ‘childbirth’ issue, but actually only 17% of these deaths occur during the labor, birth or immediate recovery phase. However, a whooping 52% occur during the 12 months after a new mother gives birth, and this number does not include suicide, which is three times greater than deaths from medical complications.
For the last century, maternity care in the US has focused intensely on pregnancy and childbirth. As a result, healthy new mothers and their neonates are discharged from the hospital after 48 hours with no scheduled follow up for the new mother until the traditional 6-week check up.
ACOG recently recommended that new mothers be first seen in the office at 3 weeks, but currently there is no formal mechanism for home visits during the first week after hospital discharge and no regular follow up after the 6 weeks visit.
The most common medical reasons for postpartum deaths include hypertension, pulmonary embolisms, infection and increasing rate of undiagnosed *cardiopathy (*car-de-op-oh-thy, i.e. seriously weakened heart muscles). Even more disturbing is the suicide rate from postpartum depression during the first year, which as I mentioned is 3 times higher than medical complications.
 According to a CDC spokesperson, some of these new mothers died because they lacked access to good health care, resulting in delayed or missed diagnoses of crucial medical problems. Serious racial disparities also exist. Black and American Indian/Alaska Native women were about three times as likely to die from a pregnancy-related cause as white women. Officials said this data suggests that the majority of deaths, regardless of when they occurred, could have been prevented by tackling these key problems.
According to a CDC spokesperson, some of these new mothers died because they lacked access to good health care, resulting in delayed or missed diagnoses of crucial medical problems. Serious racial disparities also exist. Black and American Indian/Alaska Native women were about three times as likely to die from a pregnancy-related cause as white women. Officials said this data suggests that the majority of deaths, regardless of when they occurred, could have been prevented by tackling these key problems.
Dr. Wanda Barfield, director of the Division of Reproductive Health in CDC’s National Center for Chronic Disease Prevention, noted that the CDC’s new analysis underscored the need for access to high-quality services, risk awareness and early diagnosis and preventing future pregnancy-related deaths. She said that by identifying and promptly responding to warning signs not just during pregnancy, but up to a year after delivery, we can save lives …”.
Postpartum care currently provided by Cal LMs:
California licensed midwives make 2 postpartum-neonatal house calls in the first few days after the birth, with scheduled office visits to see the new mother and baby at 2 and 6 weeks.
Proposal for expanding postpartum scope of practice and adding a relevant educational module to the LMPA
I’m proposing to extend the formal scope of practice for licensed midwives to include the first 12 months postpartum and to add an education module for recognizing the signs and symptoms of pulmonary embolism, cardiopathy and postpartum depression to the educational criteria for LMs.
 Many midwives, myself included, already provide expanded postpartum care or what we call Second Nine-Month Care. At the 6 weeks visit, I offer to see the new mother at 3, 6, and 9 months. This could easily be expanded to include a one-year visit.
Many midwives, myself included, already provide expanded postpartum care or what we call Second Nine-Month Care. At the 6 weeks visit, I offer to see the new mother at 3, 6, and 9 months. This could easily be expanded to include a one-year visit.
An additional benefit of extending midwifery care to one year postpartum is that healthcare organization like Kaiser, community clinics and obstetrical groups could formally employ LMs to provide extended postpartum care as home visits for new mothers just released from the hospital and 30-minute offices at 3, 6, 9 and 12 months.
Thank you for your time and I hope you will favorably consider my proposal.
{ 0 comments }
~ faith gibson ~
written 2002, revised Sept 2007, posted on FG.org Jan 2020
 I am one of the few individuals in either the midwifery community or the employ of the Medical Board who has been involved full-time in the legal and legislative issues of California midwifery before, during and after the passage of the 1993 LMPA.
I am one of the few individuals in either the midwifery community or the employ of the Medical Board who has been involved full-time in the legal and legislative issues of California midwifery before, during and after the passage of the 1993 LMPA.
I have done extensive academic research on the history of the medical practice act and midwifery licensing laws in California and maintain an archival library on the topic.

Senator Lucy Killea, author of SB 350 ~ the Licensed Midwifery Practice Act of 1993 (LMPA)
The major sources of documentation quoted here are California medical practice legislation from 1876 to 1993, microfilm copies of state legislature bill sets, official letters of legislative intent, daily newspapers of the era, medical periodicals and the copious records provided by the Directories of Licentiates published yearly by the Medical Board.
I’ve been personally present at virtually 100% of the public meetings and major events relative to the implementation and administration the midwifery licensing program. I am called upon by Legislative staff, MBC staff members and attorneys for information about customary practices of direct-entry midwifery or to help determine the logic of the administrative issues relative to licensing.
I administered a professional liability group policy for community-based midwives in three states between 1998 and 2001. More recently I was the lead author of the official Standard of Care for California LMs adopted into regulation by the Medical Board under the authority of SB 1950.

Senator Liz Figueroa, author of midwifery amendments SB 1479, SB 1950 and SB 1638
In July 2004, I requested and Senator Figueroa agreed to carry legislation creating MBC Midwifery Advisory Council, which was accomplished by SB 1638 in 2006. This was the 3rd time that Senator Figueroa passed amendments to the LMPA. Currently I am the Chair of the MBC’s Midwifery Advisory Council.
I was an L&D and ER nurse for 17 years before I cross-trained into midwifery. Due to the ‘poison pill’ in the Nurse Midwifery Practice Act (mandatory obstetric supervision), I chose not to become a certified nurse midwife (CNM) and instead trained as a non-medical midwife. I am a nationally certified professional midwives (CPM) under the North American Registry of Midwives and California licensed midwife #041. I practice under the regulatory authority of the Medical Board.
As an LM, I currently provide home-based birth services and hospital-based support services, thus I am personally familiar with the issue of physician supervision. As with all other licensed midwives in the state who attend planned home births (PHB), I myself do not have a physician supervisor.
Like Ms. H, I have informal relationships with a few obstetricians who, on occasion, permit me to consult with them and who collaborate with me relative to medical evaluation or hospital care of my clients. Midwives have always had informal backup arrangements for their clients, which are identified antepartum and documented in the client’s record.
As for the issue of safety and efficacy of PHB, it must be noted that a consensus of the scientific literature identifies the physiological management of normal birth
(a) in essentially healthy childbearing women
(b) as provided by experienced midwives in independent birth centers and client homes
(c) with access to appropriate obstetrical services for complications
(d) to be equally as safe as obstetrically-managed hospital births for this same healthy cohort
These studies assign all complications and mortality to the midwifery cohort, even though the mother may actually have transferred to the hospital at the start of labor, the intrapartum was medical managed and the birth attended by an obstetrician.
As for efficacy of PHB care, the scientific literature identifies a dramatic reduction in the number of obstetrical interventions by a factor of two to ten times, with a CS rate under 4%, while preserving the same level of perinatal wellbeing. When maternity care for healthy women adheres to the principles of physiological management, a non-medical setting is as safe as any other location, with the added bonus of conserving expensive medical resources. [encl #1]
Institutional Memory For MBC & Midwifery
Institutional memory is a particular issue in regard to the MBC agency staff person assigned to the midwifery licensing program, as there have been 8 different employees in the first eleven years of the program, starting with Tony Arjil in 1994. The position was sequentially filled by Gloria Maceus, Gizzelle Biby, Kim Marquart, Teri Kizer, Susan Lancara and Herman Hill. Mike McCormick is currently assigned to the staff position. {note-2-self — update the list, ck. names and spelling for Cheryl Thomas, Robin Cook, Kim Kirkmeyer,
During the first decade of the midwifery licensing program, the job went unfilled for long stretches. Employment of each of the six initial employees lasted only 6 to 18 months. This high turnover and lack of continuity resulted in much confusion for both the MBC staff and for California midwives. In addition, there have been four different executive directors since 1994.
In light of these circumstances, I offer the following background facts as a source of “institutional memory”. The majority of individuals who worked for the midwifery licensing program or participated in the Midwifery Licensing Implementation Committee are either still working for or are available to the MBC and should be able to corroborate the information provided by me. Audio tapes and written transcripts also exist for much of the material relative to the Midwifery Implementation Committee.
Historical Background ~ Original 1917 & 1949 Midwifery Legislation
State certified non-nurse midwifery already has a long and honorable tradition, going back to 1917, when the first midwifery certification law was passed. The original 1917 midwifery amendment was written entirely by physicians, a time before women had the right to vote and without the knowledge or input from the public or practicing midwives of the era.
The1917 physician-authors of the original midwifery statue were primarily concerned with setting criminal penalties for midwives who engaged in the unauthorized practice of medicine. The title of the 1917 enactment reads:
“to add a new section …relating to the practice of midwifery, providing the method of citing said act and providing penalties for the violation thereof”.
This idea is best captured by the idea of ‘girl toys’ and ‘boy toys’ –the male profession of medicine want to be sure the female profession of midwifery did not encroach into their territory and use any of the ‘boy toys’ associated with the practice of medicine. This was a strictly unilateral undertaking, as the girl toys of midwifery were not likewise protected from the encroachment of the medical profession.
However, once passed, midwives were generally compliant with all aspects of its provisions. Unfortunately, earlier forms of the Medical Board (i.e., the Board of Medical Examiners) were not equally interested in being cooperative with the midwives of that era.
In the 73 years of state regulated non-medical midwifery practice (1917 to passage of the LMPA in 1993) there was a total of 217 California certified midwives. Only 3 disciplinary actions are recorded in the Directories of Licentiates from 1918 to 1950 and all three are for overstepping the identified non-surgical scope of midwifery practice established in AB 1375.
State certified midwives Marie Caron (FX-83 -1918), Elena Rinetti (FX-97 -1918) and Caterina Reorda, a graduate of the Royal University of Turin, Italy (F-58 -1925) all had their licenses revoked or suspended for unprofessional conduct, citing “illegal operation” as the cause of action.
It appears from the various documents of the era, including the Directories of Licentiates, that no midwives were ever prosecuted for the illegal, unauthorized or uncertified practice of midwifery, either before or after the passage of the original 1917 provision, and through out the balance 20th century until the Bowland case in 1974 — a total of 97 years (1876-1973).
In 1949, at the request of the Board of Medical Examiners, a bill was passed (SB 966) that repealed the application process for midwifery certification (Article 9) and eliminated the midwife classification from the list of certificates issued by the BME. The reason cited was a lack of interest in midwifery and the opinion that “midwifery was a dead class”.
In the 32 years following the original passage of the 1917 midwifery provision, a qualifying midwifery training program in the state of California was never approved by the Medical Board. This meant that California residents were unable to meet the criteria for licensing, unless the relocated to another country for training.
The midwifery provision did not stipulate any courses in professional midwifery itself, but rather mandated that midwifery students complete the same classes in anatomy, physiology, hygiene and sanitation and a 165-hour course in obstetrics taken from the medical school curriculum for physicians and drugless practitioners’ educational standards. Ironically, while mandating the same medicalized education as physicians, the provision itself forbid licensed midwives to utilizing the medical skills taught to them in these classes.
Because there were never any Board approved midwifery training programs, the only source for new applicants were either medical students that had completed the obstetrical portion of a medical school curriculum or foreign-trained immigrants – primarily Japanese – who were licensed by reciprocity from one of Japan’s 27 midwifery schools. By far, the largest categories of California certified midwives were Japanese and Italian immigrants.
When one considers that the US was at war from 1941 to 1945 with both Japan and Italy and that the Japanese population of California was interned out of state for the duration of WWII, it is not surprising that there were only 9 applications for a midwifery license in the entire decade preceding the request by the Board to eliminate the licensing program. The last two applications in 1947 and 88 (both denied) were for licensing by reciprocity from Japan and Italy.
The legal impact of SB 960 on the practice of already certified/licensed midwives was nil and the 46 midwives who held valid licenses at the time were unaffected. The midwifery provisions defining the extent and the non-medical character of midwifery (Section 2140) and those concerning penalties for unprofessional conduct were left intact (section 2400-08). No criminal penalties for lay or uncertified practice were stipulated in this revision. The last state-certified midwife under Article 24 declined to renew her license in 1990.
After the repeal of the category of ‘midwife certificate’ —1949 to 1993 — no licensing was available in California for non-nurse midwives. However, the practice of traditional midwifery was not statutorily prohibited in either the original 1917 statute or the 1949 repeal of the direct-entry midwife application, i.e., no provision in the original midwifery licensing law or its 1949 amendment created a public offense defined as ‘practicing midwifery without a license’. Under democratic forms of government, what is not expressly outlawed is legal.
A convention of all form of government licensing is exclusive entitlement in both title and scope of practice in the domain of one’s license. Unfortunately, midwives licensed under the 1917 provision did not enjoy this protection. Unlike the professions of medicine, nursing, dentistry, chiropractic and other allied healthcare disciplines, midwives have never been granted exclusive entitlement to their scope of practice as the regulated profession of midwifery.
The original midwifery statue was primarily concerned with setting criminal penalties for what physicians defined as the illegal practice of medicine by midwives, that is, the use of drugs and “instruments” (i.e., primarily obstetrical forceps). The 1917 midwifery provision of the MPA prohibited the use by midwives of any “artificial, forcible or mechanical means”. It also prohibited the use of instruments to penetrate or severe human tissue beyond the cutting of the umbilical cord.
These activities were specifically defined in regard to childbirth as an unauthorized practice of medicine and thus illegal if performed by a midwife (except as a medical emergency under section 2063). As for the entitlement issue, these same physician-authors quietly side-stepped the complexities that licensure created by not including exclusive entitlement language for midwives in the 1917 provision.
One practical reason for not addressing this issue is that physicians and midwives share a common patient base – that is, both provide normal maternity care to healthy women. Were midwives to have been granted exclusive entitlement to their own scope of practice, it would have created the crime of the ‘unauthorized’ or illegal practice of midwifery.
Physicians who also wished to provide normal maternity care to healthy women could be charged with the unlicensed practice of midwifery. This would have required that physicians either become additionally trained and licensed in the discipline of midwifery or that an equivalent midwifery curriculum be incorporated in the medical school education, thus granting physicians an exemption to the midwifery licensing law.
Between 1949 and 1993 the public demand for midwifery care continued on as before, though statistically insignificant as compared to obstetrical care. The 1949 passage of SB 966 repealing the certificate classification of ‘midwife’ withdrew the opportunity for future midwives to become state-certified “professionals”, thus demoting them to the generic classification of “lay” practitioners deprived of professional rights such as employment opportunities, teaching positions and receipt of third-party payments.
In the course of my research I could find no records indicating that the Board of Medical Examiners ever viewed the lay practice of midwifery as an illegal activity through out the 19th and 20th century until the Bowland case in1973.
Continued in Part 2 ~ Contemporary Midwifery Licensing:
Easy to share link –> http://tinyurl.com/y3yeju59
An illegal action by California’s Sutter Health {Oct 2018} defined by NAFTA as an “disguised restriction of services“
An unfair & illegal business practice by California state law B&P Code 17200 – 17209
Below is:
- Transcript of an official Obstetrical Consent Form dated 10/08/2018
- Politician Action Plan for California Residents
In addition to the lawful documentation of patient consent for obstetrical services, the Sutter Health document goes on to informs their maternity patients that OBs covered by Sutter Health will withdraw their professional services whenever they find out that parents are planning an out-of-hospital/home birth.
@@@@@@@@@@
Sutter Health
Sutter Gould
Medical Foundation
OBSTETRICAL CONSENT FORM
1400 E. Briggemore Ave
Modesto, CA 95355
Larry Erickson, MD
Jon Post, MD
Masid Liva, MD
WhitneyLaciair, DO
Wilson Sava, MD
Eduardo Malvin B. Laguna Jr, MD
I ________________, understand and agree that one of the above aed physician will deliver y baby. The physician on-call will normally deliver after hours and on weekends.
I also understand that the prenatal fee quoted includes only the physician’s fees for prenatal office visits, normal vaginal delivery, and postpartum care for two month after delivery. Our fees do not include laboratory fees, pap smear, medication and injections, colposcopy and cervical biopsy, genetic studies, ultrasonography, non stress and stress tests internal and external fetal monitoring during labor , circumcision of infant, Cesarean section, assists fee for sutry, postpartum tual ligation, dilatation and curettage or in-office pregnancy test.
This list is comprehensive but not necessarily all inclusive.
I understand and agree that one of the above named Physicians will deliver my baby. The physician on call will normally deliver after hours and on weekends.
I also understand that the prenatal fees quoted includes only physician fees for prenatal office visit, normal vaginal delivery and postpartum care for 2 months after the delivery.
Our fees do not include laboratory fees pap smear medications and injections colposcopy and cervical biopsy genetic studies Ultra sonography non-stress and stress test internal and external fetal monitoring during labor circumcision of infant cesarean section assistance fee for surgery postpartum tubal ligation dilatation and curettage and in office pregnancy test.
{{The following content in the original document is a single paragraph. However, I have separated each of the four sentences to clearly identify the illegal anti-PHB statements constitute an unlaw and “disguised restriction of services”relative to midwifery care.}}
Additionally, I have been informed that Sutter Gould Medical Obstetricians do not support delivery at home because of the risks to both the mother and the baby are markedly increased when babies are born at home.
Planned home births result in double the infant death rate, lower apgar scores, higher maternal bleeding and higher risks for needing blood transfusions compared to women who plan on delivering their babies at the hospital.
I am aware that my delivery will take place at the hospital with which my insurance is contracted. Most insurance companies do not cover home birth.
If I plan to birth outside of the hospital setting, I will inform my doctor my plans immediately.
I understand that I will need to transfer my care to another doctor in a different Medical Group if I plan on delivering my baby outside of the hospital.
I understand that it is my responsibility to know whether or not my insurance company requires prior authorization for delivery if so I will let the assistant know in order for them to obtain prior authorization.
Patient signature __________________
Witness ________________________
@@@@@@@@@@@@@@@@@@@
 Political Action For California Residents:
Political Action For California Residents:
Below are simple, step-by-step Instructions for writing a one (or at most, 1 1/2) page letter to California’s new insurance commissioner, Ricardo Lara.
I double-dare every single LM on the Google group email to write a letter. I certainly plan on doing so myself.
Letters should include a “cc” at the bottom, noting that copies of your letter and accompanying documentation are also being sent to the Medical Board of California and California Association of Licensed Midwives (CALM).
This notifies Commissioner Lara (via senior staff who reads the mail), that this issue is also being brought to the attention of the MBC and the state organization for California licensed midwives.
I encourage mothers and midwives living in the Sacramento to also “cc” the Sacramento Bee and likewise forward a of their letter to the newspaper. (address also below)
If CALM is currently working with a midwifery-friendly State Legislator, his or her senior assistant should get a copy of Sutter Health’s document and be informed about this grass-roots letter-writing campaign.
 Where to begin:
Where to begin:
(1) Copy the contents of this Sutter Health OB consent form into a WORD document and then print it out.
(2) Compose a one- (or 1 1/2) page cover-letter using this or a similar template for communicating with legislators and state regulators:
After typing the date, your address and that of the California DCA ~ Insurance Commissioner (full address below), use a “Regarding” (i.e., RE:) that quickly identifies the topic, some version of:
RE: Unlawful actions by Sutter Health targeting out-of-hospital birth services:
Enclosed copy of Oct 2018 Sutter document that refuses to provide OB prenatal care or childbirth services to pregnant women insured under the Sutter Health plan who are receiving concurrent care for a planned OOH birth, from a California licensed professional midwife (CNM or LM)
Then identify yourself in a sentence that includes (a) your age and gender, (b) length of California residency, and (c) your demographic category — concerned citizen, childbearing woman, parent, grandparent, midwife or other HC professional, and/or community-activist, etc.
In a sentence or two, explain why you believe Sutter Health’s policy is anti-competitive {{ California’s “Unfair Competition” law is B&P Code 17200 – 17209}} and violates the law and that you also find Sutter’s policy offensive on ethical and/or constitutional grounds. (see definition of B&P Code 17200 below that would apply to statements and scare tactics used in the OB consent form.
(Examples: That Sutter’s stated policy drastically misrepresents the facts in relation to safety; the right of self-determination that applies to all mentally-competent adults regardless of gender, high CS rate associated with hospital-based obstetrics for healthy childbearing women and its associated dangers including significant increase in maternal morbidity and mortality, the unaffordability for those without health insurance or who have high co-pays, etc )
 You can provide two examples, one that is more complex and includes informative statistics (quotes from MANA, LMAR, Childbirth Connection, “Listening to Mothers Survey“, other published studies, etc) and a second topic that addresses issues such as the cost of EFM in light of the scientific literature, including ACOG’s 2003 Task Force on Cerebral Palsy and other studies that concluded (Female Patient April 2011):
You can provide two examples, one that is more complex and includes informative statistics (quotes from MANA, LMAR, Childbirth Connection, “Listening to Mothers Survey“, other published studies, etc) and a second topic that addresses issues such as the cost of EFM in light of the scientific literature, including ACOG’s 2003 Task Force on Cerebral Palsy and other studies that concluded (Female Patient April 2011):
“Despite the widespread use of EFM, there has been no decrease in cerebral palsy. … meta-analysis of randomized control trials has shown that EFM has no effect in perinatal mortality or pediatric neurologic morbidity.2 However, EFM is associated with an increase in the rate of operative vaginal and cesarean deliveries.1”
State that your letter represents a formal request to the California Department of Insurance investigate your complaint against Sutter Health for violation of B&P Codes 17200-17209.
End with something like:
“Thanking you in advance for attending to my complaint. I’m looking forward to a reply from CDI within the next 60 days
At the very end (after your signature), be sure to type in the lower case letters “cc”, and list the agencies and organizations that you will be mailing xeroxed copies of both your letter and the Sutter Health OB Consent document.

Don’t forget to email a copy to Rosanna Davis, president, CALM.
MAILING ADDRESSES & REFERENCE MATERIALS
B&P Code 172000 @@@@@@@@@@@@@@@@@
California’s “Unfair Competition” Law. (Business & Professions Code 17200 – 17209) California’s “unfair competition” law prohibits false advertising and other anti-competitive practices. Lawsuits can be brought by either consumers or by businesses that have been damaged by a competitor’s unfair actions.
California Business & Professions Code §17200 prohibits any “unlawful, unfair or fraudulent business act or practice” and any “unfair, deceptive, untrue or misleading advertising.”Jul 12, 2017
EFM @@@@@
 Quotable materials on the utter failure of policy mandating use of continuous EFM on healthy women with normal pregnancies and it’s high human and economic costs
Quotable materials on the utter failure of policy mandating use of continuous EFM on healthy women with normal pregnancies and it’s high human and economic costs
http://tinyurl.com/y3ty2392 ~ The False Association btw the routine use of continuous electronic fetal monitoring (c-EFM) to prevent Cerebral Palsy, Maternal Pelvic Floor Damage & Protect OBs from Lawsuits ~ Part 1 (of 3)
@@@@@ ADDRESSES for CDI & MBC @@@@@@@
California Department of Insurance
Contact Us
Hotline Telephone Numbers
| Consumer Hotline…………………………………. | 1-800-927-4357 (HELP) 1-800-482-4833 (TTY) or send us an email |
| Licensing Hotline………………………………….. | 1-800-967-9331 |
| California Low Cost Automobile Program.. | 1-866-602-8861 |
CDI Headquarters Offices
Sacramento Office
300 Capitol Mall, Suite 1700
Sacramento, CA 95814
San Francisco Office
45 Fremont Street, 23rd Floor
San Francisco, CA 94105
Los Angeles Office
300 South Spring Street, South Tower
Los Angeles, CA 90013
@@@@ MBC @@@@
 THE MEDICAL BOARD OF CALIFORNIA
THE MEDICAL BOARD OF CALIFORNIA
2005 EVERGREEN STREET, SUITE 1200
SACRAMENTO, CA 95815
Email Us Please include your full name and, if applicable, your license number so we can better assist you
webmaster@mbc.ca.gov
@@@@@ Sac Bee @@@@
Main Office
The Sacramento Bee
2100 Q. St.
Sacramento, CA, 95816
Telephone:
(916) 321-1000
www.sacbee.com.

{ 0 comments }
https://tinyurl.com/ydcmxlkv
 ACOG Committee Opinions #166 and #214, the 2000 Amendment (SB 1479) to the LMPA of 1993 and the midwifery Standard of Care ~
ACOG Committee Opinions #166 and #214, the 2000 Amendment (SB 1479) to the LMPA of 1993 and the midwifery Standard of Care ~
Limitations imposed by AB 1308 in 2013 that repealed the standard of care and statutorily denied ‘patient autonomy’ and ‘self-determination’ to essentially healthy childbearing women
The Standard of Care for California Licensed Midwives (SCCLM) was legislatively authorized by Senate Bill 1950 in the year 2002, adopted by the MBC in September 2005 and formally approved and published as a legally-binding regulation by the Office of Administrative Law (OAL) in March 2006.
The licensed midwife who compiled the final version of the Standard of Care in 2004 used ACOG Committee Opinions #166 and #214 as a guide for developing the legal principle that defined childbirth-related consent (i. e., that no one can touch or treat a competent adult without the adult’s informed consent) –when developing Section V of the Standard – The Responsibilities of the Licensed Midwife and the Client’s Right of Self-determination.
The result was these two short statements that defined the ethical and legally-binding relationship between professional midwives and California childbearing families from March 6th, 2006 to January 1st, 2014.
They read:
Responsibilities of the Licensed Midwife
With respect to the care of a client with a significant risk factor as identified by the client-selection criteria in section IV, other science-based parameters or physical examination, the licensed midwife shall recommend that her situation be evaluated by a licensed physician who has current training and practice in obstetrics.
Client’s Rights to Self-Determination
In recognition of the client’s right to refuse that recommendation, as well as other risk-reduction measures and medical procedures, the client may, after having been fully informed about the nature of the risk and specific risk-reduction measures available to her, make a written informed refusal.
If the licensed midwife appropriately documents the informed refusal in the client’s midwifery records, the licensed midwife may continue to provide midwifery care to the client consistent with evidence-based care as identified in this document and the scientific literature.
In addition to the ACOG Opinions, the “Intent” language in SB 1479 was also used to craft this ‘state of the art’ description of the legal duties of the LM and the legal rights of the client. SB 1479, which is the second amendment to the LMPA, provided a ‘legislative remedy’ that addressed a problematic ruling in a California Supreme Court ‘Stare Decisis” case in 1976.
 In Bowland v. Municipal Court, the Supreme Court noted that California childbearing women had no established right to make decisions about the type of care they received during pregnancy and childbirth. The opinion went on to say that the State Legislature had “never gone so far” as to acknowledge that, as a class, healthy childbearing women had the right to choose “the manner and circumstances of normal childbirth”.
In Bowland v. Municipal Court, the Supreme Court noted that California childbearing women had no established right to make decisions about the type of care they received during pregnancy and childbirth. The opinion went on to say that the State Legislature had “never gone so far” as to acknowledge that, as a class, healthy childbearing women had the right to choose “the manner and circumstances of normal childbirth”.
In the year 2000, the second amendment to the LMPA addressed this issue by legislatively acknowledging, for the first time, that essentially healthy childbearing women had, in essence, a right to choose the manner and circumstance of their normal childbirth. This amendment to the LMPA put into black-letter law the relevant theories of “Patients’ Rights” in regard to normal childbirth.
This identifies the lawful right of competent adults to receive relevant information about their health status and any possible, probable or diagnosed medical conditions or complications; after due consideration of these facts, an adult can either consent or decline treatment and other medical services or negotiate a compromise arrangement. This human right is not negated simply because of one’s female gender and pregnant condition, even if an obstetrician sincerely believes that he or she knows better than you what is best for you.
As referred to earlier, Gabee’s “Obstetrics: Normal and Problem Pregnancies” (2nd edition), chapter 42 on the “Legal and Ethical issues in Perinatology” defines “consent” in relation to healthcare as:
“A fundamental premise of Anglo-American law … that no one can touch or treat a competent adult without the adult’s informed consent.” p. 1342.
 Relevant Excerpts of AGOG’s Ethics’ Committee Opinions:
Relevant Excerpts of AGOG’s Ethics’ Committee Opinions:
ACOG’s Committee Opinion #166 on “Informed Refusal” notes that:
“Almost universally, informed consent laws have been liberalized … from the relatively paternalistic “professional or reasonable physician” standard to the “materiality of patient viewpoint” standard.
In the “patient viewpoint” standard, a physician must disclose … the risks and benefits that a reasonable person in the patient’s position would want to know in order to a make an “informed” decision.”
ACOG Opinion #214 on “Patient Autonomy: The Maternal-Fetal Relationship” states that:
- … medical knowledge has limitations and medical judgment is fallible. Existing methods for detection … are not always reliable indicators of poor outcome, and there is often insufficient evidence for risk-determination or risk-benefit evaluation
- The role of the obstetrician should be one of an informed educator and counselor, weighing risks and benefits ….and realizing that tests, judgment and decisions are all fallible.
- Abiding by the patient’s autonomous decision will provide the best care for the pregnant woman and the fetus in most circumstances.
- In the event of an emergency … the obstetrician must respect the patient’s autonomy, continue to care for the pregnant woman, and not intervene against the patient’s wishes regardless of the consequences.
ACOG Committee Opinion #214 also identifies serious negative consequences when a patient’s autonomy is violated, stating that:
- A woman is wronged and may be harmed, whether physically, psychologically or spiritually.
- The patient’s subsequent loss of trust in the healthcare system may reduce the health care provider’s ability to help her and may deter others from seeking care.
- There may be other social costs associated with this violation of individual liberty.
Senator Liz Figeroa, author of the first 3 amendments to the LMPA ~SB 1479 (2000), SB 1950 (2002, and SB 1638 (2006),
SB 1479 included a “Legislative Intent” section that acknowledged, as a matter of California state law, that childbirth was a normal aspect of biology and not a medical disease. It also identified physiological management — the supportive, non-interventive practices that are a fundamental aspect of community-based midwifery as a non-allopathic discipline that is clearly distinct from obstetrical medicine.
According to the California Legislature,
the midwifery model of care includes:
- informed choice
- continuity of individualized care
- sensitivity to the emotional and spiritual aspects of childbearing
- monitoring the mother throughout the childbearing cycle including
her physical, psychological, and social well-being - providing individualized education, counseling, and prenatal care
- continuous hands-on assistance during labor and delivery
- postpartum support
- minimizing technological interventions
- identifying and referring women who require obstetrical attention
 AB 1308 ~ Deletions and Additions to the LMPA
AB 1308 ~ Deletions and Additions to the LMPA
as they affect the California Licensed Midwife’s scope of practice and Standard of Care for Midwives
( Note – the excerpt below is just a section in a 14-page document; there are many other, usually small deletions and additions throughout the Standard of Care/Practice Guidelines as posted on the MBC’s website)
@@@@
In 2013, the original “Standard of Care of California Licensed Midwives” (SCCLM) was repealed by AB 1308, including Section V.
In December of 2013, the Medical Board of California (MBC) formally deleted the SCCLM from the Board’s website, because AB 1308 was to take effect on the 1st of January 2014.
However, at the December 5th meeting of Medical Board’s Midwifery Advisory Council, its members unanimously requested that the Medical Board make an unofficial version of the SCCLM available on the Board’s website as a helpful reference for California LMs.
The MBC agreed to develop an informal version that was to be known as “Practice Guidelines”. These new ‘Guidelines’ reflected the many deletions and additions in AB 1308, including drastically altering the Responsibilities of the Licensed Midwife and deleting in toto the Client’s Right of Self-determination (gone like the wind!)
A senior member of the MBC staff (Curt Worden) explained to the Advisory Council and members of the public that the informal ‘Guidelines’ did not have any statutory authority, and therefore would not have any legal standing. This meant the principles it described and its recommendations of “best practices” for community-based midwifery can no longer be used to defend a midwife’s practice in a disciplinary hearing or other legal situations.
–>KEY to legislative changes in the wording in the Standard of Care/Practice Guidelines as it was crafted by MBC staff at Dec 5th, 2013 Midwifery Council meeting
A strike-thru identifies mandatory deletions in the original (SCCLM) document by the MBC’s staff in their effort to be sure the new “Practice Guidelines” were in compliance with AB 1308
RED = additional restrictions based on AB 1308.
May 2014
PRACTICE GUIDELINES
FOR CALIFORNIA LICENSED MIDWIVES
@@@@
V. RISK FACTORS IDENTIFIED DURING THE INITIAL INTERVIEW OR ARISING DURING THE COURSE OF CARE
DELETED VERSION, replaced by AB1308 –> Responsibility of the Licensed Midwife
With respect to the care of a client with a significant risk factor as identified by the client selection criteria in section IV, other science-based parameters or physical examination, the licensed midwife shall recommend that her situation be evaluated by a licensed physician who has current training and practice in obstetrics.
DELETED, no replacement by AB 1308 –> Client’s Rights to Self-Determination
In recognition of the client’s right to refuse that recommendation, as well as other risk-reduction measures and medical procedures, the client may, after having been fully informed about the nature of the risk and specific risk-reduction measures available, make a written informed refusal.
If the licensed midwife appropriately documents the informed refusal in the client’s midwifery records, the licensed midwife may continue to provide midwifery care to the client consistent with evidence-based care as identified in this document and the scientific literature.
Post-AB 1308 VERSION of the: “Responsibility of the Licensed Midwife”
With respect to the care of a client who deviates from a normal pregnancy as identified by the client selection criteria in section IV or other science-based parameters, the licensed midwife informs the client that her situation must be evaluated by a licensed physician who has current training and practice in obstetrics and gynecology.
If the physician determines that the client’s condition or concern has been resolved such that the risk factors presented by a woman’s disease or condition are not likely to significantly affect the course of pregnancy, the licensed midwife can continue to provide primary care.
The client should further be informed that unresolved significant risk factors will limit the scope of the midwife’s care to concurrent care with a physician, regardless of whether the woman has consented to care or refused care by a physician. {!!!}
It is recognized that the client has the right to refuse the recommended referral; however, pursuant to the law, the licensed midwife cannot continue care. {!!!}
The licensed midwife will document refusal of the referral in the client’s record. (bold emphasis added)
Faith’s COMMENTARY:
In a side-by-side comparison, this material speaks for itself — AB 1308 is illogical, paternalistic and profoundly unconstitutional. AB 1308 is out of integrity with ACOG’s own practice standards and ethics, as Committee Opinions # 166 and #214 attest to in the clearest terms.
AB 1308 throws the rights of childbearing under the bus, an act ACOG itself acknowledges in Opinion #214 “, as a “violation of individual liberty”.
 AB 1308 was negotiated by lobbyists for the surgical specialty of obstetrics and gynecology. The product of those negotiations is an unconstitutional double standard by the ‘special interests’ of organized medicine and it’s political machine that continues to specifically violate the individual liberty of healthy childbearing families while acknowledging the concepts of ‘informed consent’ and ‘individual liberty’ in relation to women who choose their own obstetrical services.
AB 1308 was negotiated by lobbyists for the surgical specialty of obstetrics and gynecology. The product of those negotiations is an unconstitutional double standard by the ‘special interests’ of organized medicine and it’s political machine that continues to specifically violate the individual liberty of healthy childbearing families while acknowledging the concepts of ‘informed consent’ and ‘individual liberty’ in relation to women who choose their own obstetrical services.
Could this “disguised restriction” on the services of midwives (generally illegal under NAFTA) also be a restraint of trade that is part and parcel of an organized campaign to eliminate, or at least disadvantage, a class of economic competitors?
I believe these quotes are more than enough to establish the validity of these observations:
*ACOG* Opinion #166 — “Almost universally, informed consent laws have been liberalized … from the relatively paternalistic “professional or reasonable physician” standard to the “materiality of patient viewpoint” standard.”
AB 1308 is specifically paternalist as defined by their very own words.
*ACOG* Opinion #166 — In the “patient viewpoint” standard, a physician must disclose … the risks and benefits that a reasonable person in the patient’s position would want to know in order to a make an “informed” decision.”
AB 1308 says in black-letter law that childbearing women who choose to receive their maternity care from a Ca LM do not have the right of “informed consent”, which also would include the right to decline unwanted obstetrical consultations without losing access to the safety net of professional midwifery care.
*ACOG* Opinion #214 … medical knowledge has limitations and medical judgment is fallible. Existing methods for detection … are not always reliable indicators of poor outcome, and there is often insufficient evidence for risk-determination or risk-benefit evaluation
AB 1308 does exactly the opposite of ACOG’s own ethical standards. Instead of admitting that “medical knowledge has limitations and medical judgment is fallible, it claims the obstetrical profession is 100% perfect, 100% of the time, and goes on to translate this irrational concept into black letter law.
AB 1308 boldly (shamelessly!) insists that obstetricians are the only appropriate decision-makers, the only people on Planet Earth that can (and should) legally determine what is “best” for childbearing women — especially those who are so foolish as choosing the care of a licensed midwife instead of an obstetrician and furthermore, are planning an OOH birth.
*ACOG* The role of the obstetrician should be one of an informed educator and counselor, weighing risks and benefits ….and realizing that tests, judgment and decisions are all fallible.
Bingo — everything discussed above, plus the idea that members of the obstetrical profession (a) don’t really like the role of informed educator and counselor — takes too much time and there is no billing code for is, so its a money loser, and (b) obstetricians (at least those who belong to ACOG) think obstetrical medicine is infallible, and that any test, judgment, or decision made by an obstetrician is likewise infallible.
*ACOG* Abiding by the patient’s autonomous decision will provide the best care for the pregnant woman and the fetus in most circumstances.
I admit to being particularly nutty about this one. ACOG Opinion #214freely acknowledges that: “Abiding by the patient’s autonomous decision will provide the best care for the pregnant woman and the fetus in most circumstances” then it turns around and sponsors AB 1308, which says in plain English:
- … the midwife must inform the client that her situation must be evaluated by a licensed physician who has current training and practice in obstetrics and gynecology.
- … informed that unresolved risk factors will limit the scope of the midwife’s care to concurrent care with a physician, regardless of whether the woman has consented to care or refused care by a physician.
- It is recognized that the client has the right to refuse the recommended referral; however, pursuant to the law, the licensed midwife cannot continue care.
In the context of AB 1308, ACOG’s ethical statements leave me speechless!
*ACOG* Opinion #214 also identifies serious negative consequences when a patient’s autonomy is violated, stating that:
A woman is wronged and may be harmed, whether physically, psychologically or spiritually.
The patient’s subsequent loss of trust in the healthcare system may reduce the health care provider’s ability to help her and may deter others from seeking care.
There may be other social costs associated with this violation of individual liberty.
I can only say “duh!”, since this is so self-evident.
Gabee’s Obstetrics’s comments on “Forced Cesareans” on page 1336-37, put the icing on this cake by saying:
“Obstetricians should refrain from performing procedures** that are unwanted by a pregnant woman. … inappropriate reliance on judicial authority may lead to undesirable social consequences, such as the criminalization of non-compliance with medical recommendations.
{** (this would include mandatory ‘evaluations’ by an OB and putting women into the position of having to choose between highly medicalized hospital services and either a lay-midwife attended or an unattended labor and birth)
In 1990, The District of Columbia Court of Appeals, in a strongly worded opinion, essentially adopted the ACOG as law, holding the decision of pregnant women must be honored in all but:
“extremely rare and truly exceptional circumstances“. (emphasis added)
How the limitations imposed by AB 1308 affect the LMPA and its previous amendments
 Unfortunately, the unjustified and unconstitutional AB 1308’s assault on mothers and midwives does not stop with the egregious violation by ACOG of its own ethical guidelines but violates the principles established in the LMPA itself.
Unfortunately, the unjustified and unconstitutional AB 1308’s assault on mothers and midwives does not stop with the egregious violation by ACOG of its own ethical guidelines but violates the principles established in the LMPA itself.
AB 1308 has turned the ‘shield’ provided by the LMPA into a ‘sword’ to be wielded by organized medicine against the best interests of women as clearly established in SB 350 and SB 1479.
The purpose and Legislative Intent of the LMPA of 1993 (SB 350 by Senator Killea) and the 2000 amendment (SB 1470 by Senator Figuera) was to provide healthy childbearing families with access to access to high-quality, affordable and acceptable (as defined by the family) maternity care.
It was my honor to personally know and converse with Senator Lucy Killea a number of times during the long effort to pass a non-nurse midwifery licensing law. Senator Killea was passionate about the need for a modern, non-nurse (and not-medically dominated) licensing system for the direct-entry practice of traditional midwifery.
In particular, Senator Killea saw this as reducing the human tragedy and preventable expense to the MediCal program caused by the high rate of premature birth often associated with the inability of low-income families to find affordable and acceptable maternity care.
California Senator Lucy Killea, author of the Licensed Midwifery Practice Act of 1993 and our heroine!
Senator Killea was equally committed to creating a rational and legal option for ‘alternative’ (i.e. traditional!) care so childbearing families would be able to receive childbirth services from professionally-trained and state-regulated licensed midwives. This would eliminate, or at least greatly reduce, the number (and associated dangers) of unattended birth.
Senator Killea passed that Olympic torch on to Senator Figueroa. SB 1479 forever eliminated the spurious idea put forth in the 1976 Bowland Decision that healthy childbearing women in California did NOT have the right to control the “manner and circumstance” of normal childbirth.
Thanks to Senator Figueroa — a talented and tireless advocate for mothers and midwives — the definitions of midwifery originally proposed by a national consumer group (Citizens for Midwifery), which identified normal childbirth as a non-medical event, allowed the legal definition of childbirth as a ‘normal’ biological function (and not a medical-surgical one) to be incorporated into California Law.
Negating the Bowland Decision is more important than many of us can imagine, as the midwives criminally prosecuted in the Bowland case were charged with violating section 2052 of the B&P Code, which is the illegal practice of medicine. This statutory language prohibits practicing or holding oneself out to practice “any system or mode of treating the sick or afflicted in this state“.
Kate Bowland, Linda Bennet, and a third midwife were arrested for offering to support a normal biological process in healthy childbearing women, but they were criminally prosecuted for “treating the sick or afflicted“. In other words, when midwives “hold themselves out” to be midwives, they are arrested for pretending to be doctors, and/or for doing something (in this case, attending a normal birth) that only MDs are legally authorized to do.
This crazy and factually inaccurate definition made the practice of non-medical midwifery a ‘crime‘ in 1973, when the Santa Cruz Women’s Health Clinic was raided and shut down, and its midwives (one of who was herself many months pregnant) carted off to jail in the middle of the night.
SB 1479 ended that archaic and illogical definition that equates tradition, non-medical midwifery to an illegal practice of medicine. Midwives still “treat” women — that is, we treat them with compassion and respect, which is not an illegal practice of anything!
 For decades to come, Senator Figueroa can personally take credit for providing all the citizens of Calfornia with this wonderful description of “The midwifery model of care”.
For decades to come, Senator Figueroa can personally take credit for providing all the citizens of Calfornia with this wonderful description of “The midwifery model of care”.
According to the SB 1479, professional midwifery care by California licensed midwives includes:
- informed choice
- continuity of individualized care
- sensitivity to the emotional and spiritual aspects of childbearing
- monitoring the mother throughout the childbearing cycle including
her physical, psychological, and social well-being - providing individualized education, counseling, and prenatal care
- continuous hands-on assistance during labor and delivery
- postpartum support
- minimizing technological interventions
- identifying and referring women who require obstetrical attention
Pssst! Pass this good news on to everyone who will listen ~ https://tinyurl.com/ydcmxlkv
~ Happy Birth Day ~
{ 0 comments }
https://tinyurl.com/ybvde6cx ~ This URL links to Parts 1. You can access Part 2 by clicking the link at the bottom of Part 1.
The story behind the 1993 Licensed Midwifery Practice Act and organized medicine’s 2013 amendment to the LMPA that irrationally restricts access to care by Ca LMs
The California Licensed Midwifery Practice Act was introduced in 1993 by Senator Lucy Killea specifically to reduce the risks that pregnant women and their unborn/newborn babies face when the mother-to-be does not receive quality maternity care and the associated complications of “no care” which includes an increase in premature births, undetected pregnancy complications for either mother or unborn baby, and the dangers of unattended births.
Whether planned or unplanned, not having prenatal care and not having a trusted and skilled birth attendant present during labor and birth drastically increases the danger to mothers and babies both.
Lack of prenatal care is associated with a dramatic increase in the rate of prematurity. Hospital caring for premature babies can be as much as a million dollars per infant and often includes expensive long-term disabilities. Treatment of newborns with respiratory-related difficulties, which is a major problem for premies, is the *very most expensive* type of hospital care — even more frequent and expensive than treating spinal cord injuries and 3rd-degree burns.
More than half of the hospital expense for pre-term babies is billed to the State’s MediCal program. Under dire circumstances, even high-income families come to depend on this state-federal program to pay for neonatal intensive care when the parents’ private insurance maxes out. Unfortunately, the problems associated with a premature birth do not end when the baby is discharged from the hospital. While the negative effects of pre-term birth fall heaviest on parents and child, there are also expensive downstream problems for our schools and other hidden or long-term costs to society.
As for the risks of unattended birth, they are obvious and also expensive, both in treasure and human tragedy.
The Legislative Intent of SB 350 was to mitigate these problems by better serving the needs of families who couldn’t find afford conventional maternity care and/or wanted to avoid the highly medicalized and interventive hospital care that is the current standard in the US. These families were seeking a reasonable, safe and lawful alternatives, including care by midwives trained to support the physiology of normal childbirth in a non-medical setting — the family’s home or free-standing birth centers staffed by professional midwives and family practice physicians.
Why Nurse-Midwifery Was/Is Not an Answer
Certified Nurse-Midwife, Kate Bowland (standing) & provider of planned home birth services in Santa Cruz County for 45 years (Yea Kate!)
Prior to passage of the LMPA in 1993, California law only legally recognized the practice of certified nurse-midwives (the Nurse-Midwifery Act of 1974). However, each CNM is only permitted to provide midwifery services if an obstetrician is willing to enter into a written contract with her to legally “supervise” them.
Unfortunately, the 1974 nurse-midwifery licensing law does not require that any California-licensed obstetrician actually supervise a nurse-midwife.
As an additional disincentive to the practice of nurse-midwifery, the legal supervisory role of obstetricians means doctors can be held liable for care provided by the nurse-midwife if there is a malpractice suit. Obviously, their professional liability insurance carriers do not allow them to do this.
The obstetrical profession has always seen midwifery as a competing profession and economic threat. So it’s no surprise that 99.99% of California obstetricians refuse to take on the onerous responsibility for one of their competitors. With rarest of exceptions, the few who do agree to supervise a nurse midwife insisted that she only attend hospital births, which required the midwife to abide by obstetrical department protocols (instead of physiologically-based practices).
Standard obstetrical protocols for hospital delivery, with the mother lying on her back on a delivery room table, buried under sterile drapes in an anti-gravitational position while trying to push her baby uphill while her obstetrician, L&D and nursery nurses, several medical students and other hospital personnel look on.
In 1976, families who were hoping to receive community-based midwifery care from a state-licensed CNM were dismayed to discover that the new law was obviously unworkable and did not allow this so these frustrated families sought out the services of lay midwives. However, if they were unable to locate a suitable birth attendant in their geographical area, they often opted for an unattended birth. This was such an obviously dangerous problem that Jerry Brown, during his first term as governor (1975-83), became personally involved in supporting a new, non-nurse midwifery licensing law.
Governor Brown’s administration described the impasse over mandatory supervision of midwives by obstetricians as “structural barriers to practice” inserted by organized medicine into the 1974 nurse midwifery bill. This prevented nurse-midwives from providing services to low-income women and families seeking alternative care, which was the major purpose of the licensing law. The nurse-midwifery law was also supposed to greatly reduce the cost of maternity care being paid by the State’s MediCal program, but the unworkable physician supervision clause rendered that useless as well.
In 1976, Gov. Brown directed the California Department of Consumer Affairs (the DCA is a state agency under the control of the executive branch) to actively support passage of a new, non-nurse midwifery-licensing law [AB 1896] as an independent discipline that was not under the control of the medical profession (which unfortunately is still the case for California nurse-midwives 54 years later).
During this period of time, three midwifery licensing bills (AB 1896, AB??, SB??) were introduced and promoted by the Governor Brown’s office and Mr. Michael Krisman, Deputy Director of the Department of Consumer Affairs**.
Unfortunately, the lobbying efforts of organized medicine were able to overrule even the direct support of Governor Brown and the DCA. Altogether, there were six attempts to pass a non-nurse (direct-entry) midwifery licensing law between 1976 and 1993 failed.
{** See the Department of Consumer Affairs’ 11-page document written by Deputy Michael Krisman September 8, 1977 entitled AB 1896 – BACKGROUND INFORMATION PAPER ~ THE MIDWIFERY PRACTICE ACT OF 1978
DCA’s pro-active support of a new mfry licensing law included creating the original “Midwifery Advisory Council” in 1981. Lay midwives (including myself) and many grassroot activists met regularly in the Capitol building in a conference room provided by the DCA to work on midwifery legislation that would allow state-licensed nurse AND non-nurse midwives (as a combined legal category) to be reimbured by MediCal when providing care to eligible low-income families.
In 1981 & 1983 public hearing were held in northern and southern parts of the State. These Alternative Birth Hearings were chaired by State Senator John Vasconcellos and Mr. Jack Winters (Editor’s note-2-self: Janet Ashford to may remember names & other details and still have newspaper clippings).
Senator Lucy ~ Author of the LMPA and Heroine to the State’s childbearing families and direct-entry midwives
When the overwhelming odds against passage of a non-nurse midwifery law are taken into account, Senator Lucy Killea’s offer to author and vigorously, personally promote SB 350 can be seen as the brave and bold move it really was. Senator Killea was a remarkable woman with an extraordinary history of public service.
During WWII she was employed by the US military in Europe as an “operative” (i.e. a spy). At the end of WWII, she and her new husband Jack Killea were the second and third people hired by then-President Harry Truman to run the newly authorized Central Intelligence Agency (CIA).
Senator Killea was also the only member of the Legislature to be denied communion by the Catholic Bishop of her San Deigo parish church in retaliation for her vote to decriminalize abortion. So her effort to find an alternative solution to the problems created by the historical domination of all childbirth services in the State by organized medicine over a period of 54 years was in line with her illustrative record of personal courage and ethical standards translated into protective public policy.
The intent of SB 350 was to professionalize non-nurse midwifery and ultimately improve maternal-infant outcomes in California. The ancillary goal of the LMPA was to reduce the State’s share of expense thru the MediCal program that was associated with a high rate of prematurity and childbirth-related complications resulting from a lack of access to maternity care and unattended births.
The LMPA passed the California Legislature unanimously and was signed into law by the governor on October 11, 1993. In 2016, there were more than 400 midwives licensed in California under the LMPA and over 3,000 babies born in non-medical settings (birth centers and family residence) under their care. **Licensed Midwives Annual Report (LMAR-2016)
SB 1479 ~ An Important & Clarifying Amendment to the LMPA by Senator Liz Figueroa
The LMPA was first amended in the year 2000 by Senator Liz Figueroa. SB 1479 stated as a matter of California state law that childbirth was a normal aspect of biology and not a medical disease. SB 1479 legally clarified the characteristics of physiological management and the supportive, non-interventive practices associated with the community-based practice of midwifery, which is a non-medical (in the sense of non-allopathic) discipline legally distinct from the allopathic practice of obstetrics.
By California law, the licensed midwifery model of care includes:
- Informed choice
- Continuity of individualized care
- Sensitivity to the emotional and spiritual aspects of childbearing
- Monitoring the mother throughout the childbearing cycle including
her physical, psychological, and social well-being - Providing individualized education, counseling, and prenatal care
- Continuous hands-on assistance during labor and delivery
- Postpartum support
- Minimizing technological interventions
- Identifying and referring women who require obstetrical attention
Hour-old baby boy in a “bunny bag” — a midwife’s invention that is a tiny sleeping bag made from cloth diapers and super absorbent microfiber fabric. It helps keep newborns warm while being held by family members, who often have a hard time keeping the baby covered and warm
In the year 2000, this amendment to the LMPA formally acknowledged the right of essentially healthy pregnant women to exercise self-determination in regard to normal childbirth. This was an affirmative response by the Legislature to a legal issue raised by California Supreme Court in the Bowland Decision.
In 1976 the Bowland Court ruled that childbearing women had no intrinsic right to make decisions about the type of care they received during pregnancy and childbirth, noting that the California Legislature had “never gone so far” as to acknowledge that, as a class, healthy childbearing women in California had the right to choose “the manner and circumstances of normal childbirth”.
It should be noted that the Bowland Count did not rule say that childbearing women couldn’t legally decline prenatal care during pregnancy or plan to have an unattended birth. They just noted that the Legislature had never affirmed a pregnant woman’s right to choose a maternity care provider that was OTHER than conventional hospital-based obstetrical providers.
The Legislative Intent of SB 1479 rectified this oversight, acknowledging that in California:
(b) Every woman has a right to choose her birth setting from the full range of safe options available in her community
(e) The midwifery model of care is an important option within comprehensive health care for women and their families and should be a choice made available to all women who are appropriate for and interested in home birth.
This provides legislative authority for the practice of traditional (i.e. non-physician) birth attendants and the choice by parents of tradition/alternative (out-of-hospital) locations.
In 2002, SB 1950 (Figueroa) mandated that a regulation be promulgated that would define a midwifery standard of care for California licensed midwives). This amendment resulted in the approval of the Standard of Care for California Licensed Midwives (SCCLM) by the California Medical Board in September 2005 and its formal adoption the Office of Administrative Law (OAL) in the regulatory code March 6, 2006.
In 2006, SB 1638 (Figuroa) directed the California Medical Board to create a Midwifery Advisory Council composed equally of Ca LMs and consumers. The Council meets 3 or 4 times a year and currently has 6 members. Advisory Council meetings are now webcast for public viewing and those videos are archived for reference at a later time by the public.
SB 1638 also mandated that the MBC develop an administrative process for the annual collections of statistics for all licensed midwives to be reported and collated by OSHPD (Licensed Midwives Annual Report) and formally reported by the Medical Board to the State Legislature each year.
Starting in 2007, the LMAR has tracked the number of families that received care from Ca LMs each year and standard maternal-infant statistical outcomes. These include the number of normal vaginal birth attended in an out-of-hospital setting, number of hospital transfers and all sub-optimal outcomes, including Cesarean deliveries and any serious morbidity within first 6 weeks and mortality. These online annual reports have been available to the public since 2010.
 I cannot stress enough that all these changes were sought out by practicing midwives and consumer groups, especially the California Association of Midwives (CAM) and California Families for Access to Midwives (C-FAM).
I cannot stress enough that all these changes were sought out by practicing midwives and consumer groups, especially the California Association of Midwives (CAM) and California Families for Access to Midwives (C-FAM).
We all worked hard and spent organizational funds to find a legislator willing to sponsor these amendments. After this critical stage was accomplished, professional and advocacy groups as the office staff of the two Legislator’s offices (special thanks to Liz Smith and Vincent Marchand in Sen. Figueroa’s office 2000-2006) We all burned the midnight oil to push these bill through.
Licensed midwives and consumer groups worked for changes in the LMPA that would mandate annual reporting by each practicing midwife, who would be required to provide a great many details about the care provided, including any bad outcomes. We believed that legislation mandating the Medical Board to host a Midwifery Advisory Counsel would dramatically improve the professional relationship between licensed midwives and our regulatory agency (MBC). Indeed, this has greatly improved relationship btw our regulatory agency and its midwife licentiates.
In an on-going effort to make midwifery the best it can be, the 1993 LMPA and its first 3 amendments allowed the profession of licensed midwifery to further fine-tuning the care it lawfully provides to childbearing families in California seeking alternative childbirth services that are lawful, safe, cost-effective and able to reduce the likelihood that the laboring woman and her newborns would be exposed to risky and unwanted medical and surgical interventions.
The problem is NOT Senator Killea’s midwifery licensing law, but the continued LACK of access to high-quality maternity care and midwifery services caused by inappropriate amendments to the LMPA sponsored by special interest groups
Whatever people may think of community-based midwifery, they should be reassured by the following facts:
The public health problems surrounding normal childbearing in California are not the result of the care by state-licensed midwives, but the preventable danger to pregnant women and their unborn babies when they don’t get regular prenatal care and are forced to chooe between the Devil and he Deep Blue Sea — eiher an unwanted hospial birth (or in some cases, an unwanted Cesarean) of have an unattended birth and attendant risks
The combination (no prenatal care-unattended labor, birth and neonatal period) has 20 to 40-fold increase in mortality of mothers and unborn/newborn babies. One study of unattended births in a religious group in Indiana identified 6 maternal deaths out of 344 births or 1 mother and 21 stillborn or newborn babies for every 57 births. (Perinatal & maternal mortality in a religious group avoiding obstetric care – Am Jour Obst Gyne 1984 Dec 1: 150(7):926-31: ~ see abstract at end of this document)
 Preventing Needless Childbirth Tragedies
Preventing Needless Childbirth Tragedies
The tragedies cited in the study above were all “preventable” deaths due to untreated hemorrhage in new mothers and untreated infection in neonates. Obviously, the basic issue in these cases was a regrettable (and I believe an uninformed) choice made by these families to eschew prenatal care and having a trained birth attendant present during labor and birth, as well as refusing to use medical and emergency services in the face of life-threatening complications.
But these high maternal-infant mortality statistics are a grizzly testament to just how successful midwifery care is at preventing such tragedies.
As attested to by the last 10 years of data collected by the California Licensed Midwives Annual Report (thank you Senator Figeroa!), we know the majority of unexpected problems associated with childbirth can be prevented or successfully managed when professionally-licensed midwives are authorized to:
- Provide prenatal care with regular risk-screening and referrals to medical services as needed
- Physically examine and evaluate the health status of the pregnant woman and her unborn fetus prior to the term onset of active labor (late pregnancy, very early labor), so those with complications can be prophylactically transferred to medical services
- Be present during the mother’s active labor, the birth of her baby and immediate postpartum-neonatal period and the 6-week of follow-up care for both mother and baby, which also includes hospital transfer and/or use of emergency medical services as needed
But starting in 1949, when the original 1917 midwifery licensing law was repealed by the California Legislature at the request of the medical community, no such safeguards were legally available in California until the passage of the LMPA in 1993. During that 44-year gap, California families had only two legally-recognized options:
(a) “no care” – i.e. no prenatal care; unattended birth; delayed access to emergency medical services when needed
(b) medicalized obstetrical care that is often experienced by laboring women and their families as similar to being in intensive care unit (ICU).
If those two extremes — “no care” and highly medicalized, expensive hospital-based obstetrical care for healthy women — met the needs of 100% of childbearing women in California, there would have been no need for the Legislature to ever create the new category of professionally-licensed direct-entry midwifery.
Unfortunately for the special interest groups who supported the status quo between 1917 and 1993, the actual facts belie any assumption these two extremes were able to meet the needs of the childbearing public or the fiscal responsibility of the State’s MediCal program to pay for the maternity care of eligible low-income families.
Compelling evidence in more recent times that a state-sanctioned category of professional non-nurse midwives was necessary is unanimous passage by the California State Legislature of the original Licensed Midwifery Practice Act of 1993 (SB 350) and three (SB 1479, SB 1950, and SB 1638 – Sen. Figueroa) of its four amendments.
As the risk of being redundant, the incontrovertible facts are both plain and simple: The presence of a trained midwife, like that of a lifeguard at the pool, always makes childbirth orders-of-magnitude safer for childbearing women and their unborn and newly born babies.
That means providing the option of professional midwifery care to low-income women, socially and religiously conservative families, ethnic groups that prefer traditional forms of midwifery care, and families that, for a great variety of valid and rational reasons, want or need an alternative to highly-medicalized hospital obstetrics. Since 1993, the answer to what otherwise would be insurmountable problems had been the LMPA.
Midwifery Licensing and its Important Contribution to Childbearing Families
Passage of the LMPA in 1993 legally acknowledged and preserved the traditional arts of midwifery within the context of modern medical science and evidence-based “best practices”. Through formal education and clinical training, over 400 California licensed midwives have had the opportunity to incorporate the historic quality of traditional midwifery care with the “best practices” of modern medicine.
If a medical problem should occur in an out-of-hospital setting (home or birth center), midwives are scientifically trained first-responders able to provide effective emergency interventions, and refer or transfer mother or baby to medical providers whenever necessary. As noted earlier, this reduces risks during pregnancy, and the frequency and severity of preventable childbirth complications, making normal childbirth in healthy women both *safer* and more cost-effective.
2013 ~ Hostile taker-over by organized medicine is a disguised restriction on midwifery services and denial-of-service to healthy childbearing women
Unfortunately, the fourth amendment to the LMAP represents a ‘hostile take-over’ — AB 1308 was sponsored by lobbyists representing organized medicine in 2013. This amendment, which was negotiated by lobbyists for ACOG, drastically reduced the scope of practice for direct-entry midwives and the number of essentially healthy childbearing women that California licensed midwives can legally provide services to.
Prior to its passage, the LMPA the scope of practice for CaLM was defined as providing routine prenatal care, risk-screening, and normal childbirth services to women with no evident medical, obstetrical or perinatal complications. Only if a pregnant or laboring woman or newborn developed a clinically significant complication did the LMPA mandate obstetrical care or transfer to hospital-based services. This logical and common sense provision of the law was fully supported by parents, midwives, the medical profession and the general public as an appropriate safety measure. Unfortunately, AB 1308 changed that for the worse.
AB 1308 also directly repealed the California Licensed Midwives Standard of Care and specifically negated our Standard of Care’s policy statement on the licensed midwife’s ethical duty to inform and recommend physician consultation in relation to all identified risk factors, and simultaneously denied the childbearing woman’s right to self-determination (i.e. Patients Rights), including the right to decline obstetrical referrals and evaluations in relation to certain risk factors.
AB 1308 eliminated the childbearing family’s right of self-determination and informed consent/refusal, while dramatically increasing the number of childbearing families that now don’t “quality” for midwifery services under the LMPA.
I believe this provision is unconstitutional under both state and federal law.
The legal theory of ‘Adherence’ ~ a shield for midwives and mothers
AB1308 this violates a legal theory described as “adherence“. This describes a logical expectation that a law or set of laws relating to the same general theme has an internal integrity. New laws or novel interpretations of provisions in an existing law that violates that integrity risk being struck down by the Courts. For example, if a law developed to protect minor children is being implemented in ways that predictably increased the level of danger experienced by minor children, those actions would be found to violate the basic intention of the law based on the theory of “Adherence’.
 The legislative intent and provisions of the LMPA and three of its four amendments all materially enhance a midwifery licensing law whose purpose is identified in the “Legislative Intent” as making childbirth safer. The LMPA was to design to achieve these goals by creating a legally-defined mechanism to professionally train and license non-nurse/direct-entry midwives. This was to make state-regulated midwives generally available to families that couldn’t afford (n0 health insurance), couldn’t find (due to geographical reasons) or didn’t believe conventional obstetrical care acceptable (due to religious, ethnic traditions, or PTSD).
The legislative intent and provisions of the LMPA and three of its four amendments all materially enhance a midwifery licensing law whose purpose is identified in the “Legislative Intent” as making childbirth safer. The LMPA was to design to achieve these goals by creating a legally-defined mechanism to professionally train and license non-nurse/direct-entry midwives. This was to make state-regulated midwives generally available to families that couldn’t afford (n0 health insurance), couldn’t find (due to geographical reasons) or didn’t believe conventional obstetrical care acceptable (due to religious, ethnic traditions, or PTSD).
All these aspects and implementation serve the intention of the LMPA to make pregnancy and childbirth safer for California families by providing prenatal care, risk screening, referral to medical services as indicated and reducing the risk to mothers and their unborn/newborn babies by eliminating unplanned home births because midwifery care was not available.
Mandatory Obstetrical Consultation and Evaluation under AB 1308
This amendment to the LMPA now requires mandatory obstetrical consultation for possible risk factors, even if this goes directly against the wishes of the childbearing woman and her family. The category of “risks” describes the possibility of a complication in the future but is not itself a present complication that requires any treatment.
The historical and contemporary standard of care as provided by midwives and other maternity care professionals has always required that parents be immediately informed about the presence and nature of any identified risk. When the risk is clinically significant, non-MD practitioners routinely recommend consultation with an appropriate medical specialist. However, parents have a legal right to decline and after carefully pondering the issue, some do. Consultation is not mandatory unless something is really unusual or abnormal and the practitioner believes it would be unethical to continue care without additional information.
Unfortunately, AB 1308 turns all this on its head. It mandates obstetrical evaluation, even when the moter-to-be objects or decline or the health issue involved would more appropriately be referred to another medical specialty (such as an endocrinologist or perinatologist).
Nonetheless, the law stipulates that the pregnant women be seen and evaluated by “a physician with training in obstetrics” before her midwife can provide additional care. Should the childbearing woman be so bold as to exercises her legally-recognized Patients’ Right to refuse any such recommendation, no Californa licensed midwife will legally be able to provide her with additional prenatal care or childbirth services.
If the client agrees to be evaluated by an obstetrician, and can both afford and find an OB in her geographical area who is willing to consult with her, this doctor has a legal duty to the mother under AB 1308 with determining if its appropriate (i.e. in his opinion safe) for the pregnant woman to have a midwife-attend OOH birth in light of the identified risk factor. Of course, this entails enormous legal liability for the obstetrician and so like the issue of obstetricians, the choice that obviously favors the obstetricians is to just refuse to see women referred by midwives.
When obstetricians do evaluate these patients, many routinely recommend against additional midwifery care, thus shielding themselves from all potential legal entanglements. Others OBs agree to examine the woman, but won’t write anything in the medical record, lest they be sued later on. However, without documentable approval by an obstetrician, it’s illegal for the client’s midwife (or any other Ca LM) to provide childbirth services to her.
The consequences of this provision of the LMPA are extremely problematic for all involved (including obstetricians). Under the affects of AB 1308, a significant number of essentially healthy women are needlessly forced into what they believe is an unnecessary (and unwanted) hospitalization and highly-medicalized childbirth under obstetrical protocols.
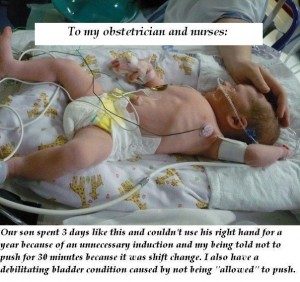 The adjacent photo is from a mother was who was still upset and angry more than a year later about unnecessary intervention in her birth and iatrogenic complications for herself and her baby. She sent this picture of her newborn in the hospital’s NICU to her obstetrician and the L&D nurses, expressing her anger and disappointment.
The adjacent photo is from a mother was who was still upset and angry more than a year later about unnecessary intervention in her birth and iatrogenic complications for herself and her baby. She sent this picture of her newborn in the hospital’s NICU to her obstetrician and the L&D nurses, expressing her anger and disappointment.
The original caption is to small to read, but it says:
“Our son spent 3 days like this and couldn’t use his right hand for a year because of an unnecessary induction and my being told not to push for 30 minutes becasue it was shift change. I also have a debilitating bladder condition caused by not being “allowed” to push.“
In the wake of AB 1308 restriction, a small but still substantial number of these women had such a bad experience with a previous hospital birth that elective hospital birth is out of the question for them. If their local midwives aren’t legally allowed to provide care to them due to restriction introduced by AB 1308, they will look for a lay birth attendant (thus re-inventing unlicensed lay midwifery!) or plan to have an unattended birth.
Up with this we cannot and should not put!
The only appropriate changes to the LMPA are ones that improve access by childbearing families or better meet their needs. while also improving the quality of professional midwifery practice. All future amendments to the LMPA must be sponsored and/or supported by consumer organization such a California Families for Access to Midwifery (C-FAM) and state midwifery organization such as the California Association of Licensed Midwives (CALM) and California College of Midwives (CCM).
All these parameters applied to SB 350 (LMPA) the 1st three amendments (SB 1479, SB 1950, & SB 1638) introduced in 2002, 2002 and 2006. But unfortunately, this was not the case for the amendment introduced in 2013.
AB 1308 directly negated many of the most important the contributions of Licensed Midwifery Practice Act, and the safeguards it provided to childbearing families by making it possible for a trained, experienced and equipped midwife to be present, and in most instances, able to prevent or successfully manage the unexpected problems associated with childbirth, especially as this applies to giving birth in out-of-hospital settings.
This must be fixed and soon.

Midwives and must consumers be (or become) informed about the history of non-nurse midwifery licensing in the State so we can explain it to others and make a compelling case to members of the State legislature.
First, we have to tell our story in order to find an author willing to carry a bill, and then we have to convince a sufficient number of legislators to support our efforts. This is especially critical for the seven Legislators who sit on the Business and Professions Committees of both chambers, a who can so easily kill a bill long before a floor vote.
To better understand the reasons why AB 1308 is not just bad policy for Ca LMs, but also unconstitutional from the perspective of childbearing families, please continue reading:
Associated Topic –> The Obstetrical Standard of Care in the US – Historically Illogical, Fundamentally & Fatally-flawed
Reference #1:
Perinatal & maternal mortality in a religious group avoiding obstetric care – Am Jour Obst Gyne 1984 Dec 1: 150(7):926-31:
This control group consists of women with the same general health and demographic characteristics that are seen in the CDC birth registration data. This is predominately healthy, white, middle-class women who had economic access to all categories of maternity care providers and settings, but in this case, purposefully choose unattended births.
Data on this group of unattended home births came from Indiana state mortality statistics for a fundamentalist religious group that rejected all forms of medical care under all circumstances – no prior diagnosis or treatment of chronic medical problems, no risk-screening of mothers during pregnancy, no prenatal care, no trained attendant during childbirth and no emergency transfer of mother or baby with life-threatening complications to a medical facility – a situation similar to rural parts of the developing world.
Out of 344 births, the unattended group had 6 maternal deaths and 21 perinatal losses. The baseline mortality rate for unattended childbirth was one maternal death per 57 mothers or MMR of 872 per 100,000 live births (92 times higher than Indiana’s MMR for the same period) and one perinatal loss for every 16 births or PNM rate of approximately 45 per 1,000.
tinyurl.com/ybvde6cx
Safe, cost-effective Childbirth in the 21st Century
Healthy childbearing women and their babies are always safer when the mother-to-be receives regular prenatal care during pregnancy, is cared for by a trained and experienced birth attendant throughout active labor, the birth of her baby, the immediate postpartum-neonatal period and initial breastfeeding and that both new mother and new baby receive appropriate follow-up care for at least six weeks after the birth.
That’s exactly what California Licenced Midwives are trained, licensed, equipped to do.
The California Licensed Midwifery Practice Act of 1993 (LMPA)
Family w/ four midwife-attended births, 1st one in the hospital, and the next three as planned home births, dad caught baby #4 (a girl) just as the midwife was arriving. See dad’s big grin holding his new daughter!) ^O^
The Licensed Midwifery Practice Act was passed unanimously by the California Legislature in 1993. Since then, approximately 50,000 families in California have had a professional midwife-attended spontaneous vaginal birth in out-of-hospital locations.
Every year more than 4,000 healthy pregnant women in our State seek alternative forms of maternity care from licensed midwives. In 2016, more than 3,000 babies were born in a non-medical setting (birth centers and family residence) under the care of California Licensed Midwives.
The best description of the role of professional midwives is to characterize them as “educated observers with emergency response capacity“. We watch, look and listen for a living, sitting quietly on the sidelines but always ready and able to spring into action, if or when the need arises.
Complications, while infrequent, can occur in any pregnancy or labor, no matter how healthy the mother or normal the pregnancy. For this reason, professional midwifery care always includes timely access to and appropriate use of medical services as an integral part of physiologically-based midwifery care, to be called on when needed to treat complications or if requested by the mother.
Should an unexpected medical problem occur during pregnancy or childbirth, midwives are trained as first-responders, able to provide effective emergency interventions, and when necessary, refer or transfer, or arrange rapid transport of mother or baby to appropriate medical services.
This greatly reduces risks during pregnancy, and the frequency and severity of preventable childbirth complications, making normal childbirth in healthy women both safer and more cost-effective. Midwives also provide emotional and social support for new parents in the months preceding and following the birth.
For women who received maternity cared from Ca LMs between 2007 and 2016, the incidence of prematurity was under 2% **. In the U.S. as a whole, preterm and premature births occur in about 12% of pregnancies and this is one of the top causes of infant death in this country.
 For women who gave birth under the care of Ca LMs during those same years, the incidence of Cesarean delivery is less than 10%**, while the US rate is 32% — a three-fold higher rate that is associated with increased infant morbidity and maternal mortality.
For women who gave birth under the care of Ca LMs during those same years, the incidence of Cesarean delivery is less than 10%**, while the US rate is 32% — a three-fold higher rate that is associated with increased infant morbidity and maternal mortality.
**Licensed Midwives Annual Report (LMAR-2007-2016).
Since 49% of the cost for all hospital births in California are reimbursed by the state-federal MediCal program, much lower rates of prematurity and surgical delivery associated with the professional services of licensed midwives save taxpayers many millions of dollars every year.
Why most Families Choose Out-of-Hospital Birth
The reasons women frequently give for choosing an OOH location for normal childbirth are:
- cultural traditions
- strongly-held religious beliefs
- economic issues
- personal preference
These reasons are relatively self-explanatory, so I won’t belabor the point. However, there are other important, but not well-known or understood reasons that I’d like to explain in some detail.
Childbirth in Women with PTSD
A small proportion of women with this debilitating form of PTSD either avoid pregnancy altogether or schedule an elective Cesarean. It’s the woman’s way of circumventing what she sees as the indignity of invasive vaginal exams during labor and other medical procedures. Hospital protocols being what they are, she doesn’t believe that her physical and emotional privacy will be adequately protected. Scheduling a surgical delivery also eliminates her fear of a loss of control and bodily integrity during a normal vaginal birth in an environment that she often sees as a quasi-public venue.
 The Intimidating Aspects of Hospitals and Hospitalization
The Intimidating Aspects of Hospitals and Hospitalization
 For the lay public (which is 99% of us), hospitals are intrinsically intimidating places. Doctors often hold our lives or those of our loved ones in their hands, but frankly, they are also busy ‘important’ people who can be brisk and off-putting.
For the lay public (which is 99% of us), hospitals are intrinsically intimidating places. Doctors often hold our lives or those of our loved ones in their hands, but frankly, they are also busy ‘important’ people who can be brisk and off-putting.
For hospital patients, these factors represent a double whammy. To be a patient is to also be in pain, afraid, sick as a dog, intimidated by high-tech medical equipment, and laying nearly naked on an ER stretcher waiting to be admitted to a hospital bed while wretching into a bowl or using a bedpan with only a flimsy curtain for ‘privacy’, thus being both helpless AND vulnerable to forces beyond our control or ability to understand.

Routine hospital Induction at 40 weeks and 4 days — the standard protocol in the U.S. based on ACOG guidelines. However, new guidelines from the recent “ARRIVE” study calls for inducing labor at 39 weeks in all pregnant women – that is 7 days BEFORE their baby is actually due. What you’re seeing in this photo is the new “norm’ for so-called ‘normal’ childbirth in America.
Families seek out midwifery care specifically to avoid the highly medicalized management of normal childbirth in the US, which they experience as similar to trying to give birth in a busy ICU.
Women in the thors of labor experience themselves as tethered to the bed by IV lines, an automatic blood pressure cuff on one arm, a pulse oximeter on a finger of the other hand, two EFM belts around their pregnant belly, with cords leading back to the electronic fetal monitor standing next to their bed, as the mother-to-be lies on her backs, watching unfamiliar members of the hospital staff come and go, while the rest of their family stands out in the hallway, waiting for the baby to be born.
The good news is that Legislative Intent of California Licensed Midwifery Practice Act perfectly matches the needs of these families for a safe and legal ‘alternative’ to a routinely medicalized hospital care and since 1993, has made this risk-reducing form of available to many thousands of California families.
SB 350 was also designed to prevent the many serious problems for childbearing women (and ultimately for society) that are associated with the category of ‘no care’, including an increase in premature births and the dangers of unattended births when state-regulated professional midwifery care is not available.
 Tell California Legislators to Vote for Stepping Stones, not Stumbling Blocks
Tell California Legislators to Vote for Stepping Stones, not Stumbling Blocks
Annulment of Midwife’s Scope of Practice and Veto Power over CB woman’s right to self-determination
In 2013, lobbyists for a special interest group — the surgical specialty of obstetrics and gynecology — approached a California legislator with what must have seemed like a logical argument for amending the LMPA. They asked for legislative provisions that:
- nullified the original scope of practice for licensed midwives
- repealed the Standard of Care for California Licensed Midwives (SCCLM)
Gateway Claims by Special Interest Groups are Neither Accurate or Objective
 This was done by making it illegal for midwives to provide care to pregnant women who had certain risk factors and eliminating the mother-to-be’s right to decide for herself whether she wanted to consult with an obstetrician in relation to these risk factors. Claims that limiting the scope of practice for midwives and eliminating Patients Rights for their pregnant women clients would make childbearing safer was neither accurate or objective.
This was done by making it illegal for midwives to provide care to pregnant women who had certain risk factors and eliminating the mother-to-be’s right to decide for herself whether she wanted to consult with an obstetrician in relation to these risk factors. Claims that limiting the scope of practice for midwives and eliminating Patients Rights for their pregnant women clients would make childbearing safer was neither accurate or objective.
As you continue to read, it will become clear that organized medicine was and remains more focused on the economic interests of the surgical specialty they represent than the well-being of healthy childbearing women who did not want or need or voluntarily consent to routine obstetrical.
The Scientific Art of Midwifery, its History, and its Future
The traditional role of midwives is that of:
“an educated observer with emergency response capacity”.
The midwife’s primary duty is to safeguard the normal physiological process while monitoring the well-being of mother and unborn baby. Midwives respond as the need arises, always being careful not to unnecessarily disturb or interfere with the normal biology of spontaneous childbirth as long as things are progressing normally.
This ‘eyes-on, hands-off’ quality of care describes a professionally-educated and clinically-experienced midwife who is physically present during active labor and able to watch and listen carefully and respond appropriately as the need arises.
This defines physiologically-based care as provided to healthy women with normal term pregnancies. The family’s informed decision to labor in a non-medical setting (parents’ home or free-standing birth center) is based on the use of time-tested physiologic childbirth practices in conjunction with the timely and appropriate use of modern medical science as needed.
Planned OOH birth — An Integration of “Plan A” and “Plan B”
Community-based midwifery care begins with a family’s informed decision to give birth in a community setting (i.e. an out-of-hospital birth) after their midwife has provided relative information about the risks and benefits normal birth in a non-medical setting for healthy women with a normal pregnancy. Midwives describe this formal “plan” as having two aspects or possible outcomes, one involving normal birth at home and the other a transfer of care to hospital-based obstetrical services.
Under the 1993 LMPA and the 2006 Standards of Care for California Licensed Midwives (SCCLM), all midwifery clients must consent, a priori, to the use of emergency medical services and/or hospital transfer for themselves or their newborn in event of a birth-related emergency. Midwives and families both see this as an appropriate safeguard to the immediate and long-term well-being of both mother and her unborn/newborn baby requires, which sometimes requires the use of 21st-century medical science as indicated.
The first part of community-based midwifery care — “Plan A” — refers a spontaneous labor at term (after 37 completed weeks of pregnancy) that progresses normally and a mother and fetus who tolerate the various stages of labor and a normal spontaneous birth at home or in a birth center without incident.
If, for any number of possible reasons, things don’t progress as expected or the parents simply request medicalized care, “Plan B” kicks in. This refers to an intrapartum transfer to a local hospital that provides comprehensive obstetrical services. Once admitted, the mother’s care is legally taken over by an obstetrician and the hospital L&D staff.
However, “Plan B” generally includes the continuing supportive presence of her midwife, who accompanies the family to the hospital and usually remains with the mother throughout the remainder of the labor and birth. After the new mother and baby are discharged, the midwife resumes her role as primary caregiver, providing regular postpartum-neonatal home and office visits for at least 6 weeks.
Some midwives also offer ‘2nd-nine-months care’ by seeing the new mother and her infant again at 3, 6 and 9 months. They provide extended postpartum care and social support for new families. This includes helping the new mother deal with the often stressful family dynamics of integrating a newborn into the household, breastfeeding issues, education about normal child development, as well as informally monitoring the mother for signs of postpartum depression that families often don’t pick-up on.
Historically, the presence of a trained midwife has always made childbirth orders-of-magnitude safer for laboring women and their unborn, newly-delivered mothers and their newborn babies.
However, it is equally true that prior to the development of modern medical science, neither midwives or doctors were reliably able to detect problems early on, before they became serious complications. When such a serious complication occurred during or immediately after childbirth, the medical profession had very little to offer.
19th-century medical doctors standing around a female patient on a dining room table being used while they perform a “blood-letting“. They have already cut into a large blood vessel in her leg and are letting her bleed into a bowl until pint or more of blood is withdrawn and discarded. Then the doctors would bleed her again (every few hours) until she either got better or died.
But the development of the new biological sciences in the early 20th century made it possible to combine the time-tested methods of physiologic childbirth as provided primarily by midwives with the best advances in obstetrical science, to create (at least in theory) the best of both worlds.
The 20th-century marriage of Traditional Midwifery and Modern Medical Science
The scientific practice of modern medicine, and the incredible ‘medical miracles’ for which it is rightfully famous, originated with the new scientific ability to prevent potentially-fatal bacterial contamination (germs and other pathogens) when performing medical and surgical procedures and to drastically reduce deadly nosocomial (i.e., hospital-acquired) infections from cross-contamination between hospitalized patients themselves and btw patients and the hospital staff.
Before these new scientific discoveries, the bio-hazard nature of hospitals made them extremely dangerous — places to avoid if at all possible — as from 20% to 90% of hospital patients died from post-op infections associated with some surgical procedures.
So it’s fitting that modern maternity care also traces its history back to the discovery of the Germ Theory of infectious disease in 1881, and the risk-reduction strategies (principles of antisepsis) developed by the British surgeon to Queen Victoria, Sir Joseph Lister. This consisted of scrupulous hand-washing, isolation of infected patients, using disinfectants and germicides to wash down hospital walls, floors, furniture, and equipment. Of particular importance in the war against bacteria was the sterilization of surgical instruments and the use of strict “sterile technique” during invasive procedures, such as vaginal exams during labor, and operations such as forceps deliveries.
We don’t usually think of the use of forceps and other invasive medical procedures associated with obstetrical care (such as manual removable of a retained placenta) as a ‘surgical operation’ but technically it is. Anytime something from the outside world (gloved hand, forceps, another instrument, a surgical sponge, etc) is introduced into a sterile body cavity, it is a ‘surgical procedure’ and requires the use of surgically ‘sterile’ technique in which everything that touches the patient must be uniformly sterile.
Three cheers for the modern biological sciences & the physician-scientists that brought this about!
British surgeon Sir Joseph Lister who in 1865 developed the “Principles of Sepsis” and “strict sterile technique” used during surgical operations. He was knighted by Queen Victoria and became her personal physician-surgeon.
Science-based Maternity Care
 What we now refer to as “maternity care”, which includes the new invention of prenatal care, wasn’t developed until early in the 20th century.
What we now refer to as “maternity care”, which includes the new invention of prenatal care, wasn’t developed until early in the 20th century.
The purpose of maternity care is to preserve the health of already healthy childbearing women. Mastery in this field means bringing about a good outcome without introducing any unnecessary harm or unproductive expense. In the US, 90% of women who become pregnant every year are healthy and 70% to 80% are still healthy and enjoying a normal healthy pregnancy with a single fetus in a head-down position nine months later.
The ideal maternity care system seeks out the point of balance where the skillful use of physiological management and adroit use of medical interventions if necessary provides the best outcome with the fewest number of medical/surgical procedures and least expense to the healthcare system and lowest rate of iatrogenic and nosocomial complications.
 The development of prenatal care in the early 20th century allowed professionally-trained midwives and doctors, for the first time, to routinely risk-screen pregnant women at each antepartum visit. This included lab work to see that the mother-to-be wasn’t dangerously anemic or infected with hepatitis or a sexually-transmitted disease.
The development of prenatal care in the early 20th century allowed professionally-trained midwives and doctors, for the first time, to routinely risk-screen pregnant women at each antepartum visit. This included lab work to see that the mother-to-be wasn’t dangerously anemic or infected with hepatitis or a sexually-transmitted disease.
The pregnant woman’s blood pressure and urine were regularly checked for evidence of pre-eclampsia and diabetes, while the unborn baby’s growth, position, and heart rate were also monitored. This preventative care allowed both doctors and midwives to detect and correct small problems before they became serious complications. Equally important, it helped to identify women with serious medical conditions, such as heart or kidney disease, or high-risk pregnancies so they could be immediately referred to an appropriate specialist.
Quality prenatal care saves the lives of mothers and babies and costs a hundred-fold less than the bills for intensive hospital care and other medical treatments for complications that could have been prevented if the mother had received good prenatal care.
During the 20th century, there has been a steady improvement in maternal-infant outcomes around the world. Many wrongly assume these improved outcomes were was the result of the highly-medicalized care for healthy women in the world’s richest countries, particularly the US.
 However, these good outcomes turn out to be the result of an improved standard of living, general access to healthcare and medical services and, in particular, the preventive use of people-intensive, low-tech maternity care.
However, these good outcomes turn out to be the result of an improved standard of living, general access to healthcare and medical services and, in particular, the preventive use of people-intensive, low-tech maternity care.
This describes the prophylactic use of eyes, ears, hands and a knowledge base by maternity care professionals, who are able to screen for risk and refer for medical evaluation as needed.
The best (and smartest!) form of maternity care integrates the principles of physiological management with best advances in obstetrical medicine to create a single, evidence-based standard for all healthy women with normal pregnancies, with obstetric interventions reserved for those with complications or if requested by the mother
This is the best ‘medicine’ for normalizing childbirth in a healthy population. @last edit 03-12-2018@
Continue to Part Two ~ The Art & Science of Modern Midwifery in California
Associated Topic –> The Physiological Manage of Normal Childbirth in Healthy Women ~ What, how, and why it’s usually not provided in hospital obstetrical departments
Why CALM, CCM & C-FAM (you too we hope) is opposed to California senate bill 457
The California Nurse-Midwives Association and the California Association of Licensed Midwives (CALM) stand together in opposition to this bill.
CALM is opposed because:
This bill, which is being promoted by anti-midwife physician groups, drastically reduces the scope of practice for both Licensed Midwives and Certified Nurse-Midwives and severely restricts access to out-of-hospital maternity care for all families in the state of California.
This bill mandates that women with potential risk factors who are planning an out-of-hospital birth must undergo a medical examination by an OB/GYN and seek their permission to remain under midwifery care. Midwives who continue to provide care without physician permission will be charged with unprofessional conduct.
This bill denies out-of-hospital midwifery care to women who have had either a cesarean section or any other previous abdominal surgery, including laparoscopy or laparotomy, for a broad range of conditions, from hernia and appendicitis to gall bladder removal.
This bill mandates that women must give birth in the hospital if they live more than 20 minutes from a hospital, which will impose even more limits on access to care for California’s rural families.
This bill mandates that women who are planning an out-of-hospital birth must be presented with so-called “informed consent” documents that are based on junk science.
SB 457 strikes down major portions of the Licensed Midwifery Practice Act of 1993. In addition, it denies essentially healthy childbearing women the right to determine for themselves *which set* of risks is most consistent with the parents’ values, goals, finances, and geographical considerations — the risks of a professionally-attended normal childbirth in a non-medical setting, OR the risks associated w/ typical obstetrical management in a hospital .
This bill strikes down the current law that gives Licensed Midwives the legal ability to obtain both routine and life-saving tests and medications, putting mothers and babies at unnecessary risk.
This bill strikes down the current law allowing Licensed Midwives to provide family planning services, denying women access to fundamental and essential reproductive health care.
This bill represents a major setback for maternal and infant health in the state of California by denying families access to care, violating their personal decision-making rights, and imposing state-mandated obstetrical care on women who are seeking out-of-hospital birth, midwifery, and other safe and cost-effective models of care.
All calls are needed, but those in Senator Bates’ district or other Republican districts are CRITICAL.
Respectfully request that Senator Bates NOT introduce anti-midwifery legislation planned for SB 457.
If you live in Senator Bate’s district, your calls TODAY are critical. Please share this alert with other midwives and midwifery supporters in your community NOW.
Senator Bates’ Sacramento Office: 916-651-4036
The message: Please respectfully request that Senator Bates NOT introduce anti-midwifery legislation planned for SB 457.
If you live in a Republican district, your calls are particularly important TODAY. Find your state senator HERE and call NOW.
The message from me, and Kate, Rox, Karen, Rosanna, Hope and many other midwives and the healthy families they serve:
Please ask your state senator if he or she would respectfully request that Senator Bates NOT introduce anti-midwifery legislation planned for SB 457.
Michael Baker FRM. CIA Operative ~ interviewed on MSNBC 04-08-2017
{ 0 comments }
Identifying the real dangers of normal childbirth in healthy women
Links to previous posts for: Part One, Part Two, Part Three
When it comes to identifying the actual dangers associated with normal childbirth in a healthy childbearing population, the American public and a majority of the medical profession frequently see dangers where there are none, while failing to identify the actual risks. This perspective sees childbirth in the human species as a defective or pathological aspect of female biology. It sees physiologically-based management as old-fashioned, inadequate, dangerous, irresponsible and all-together a bad idea.
As a result, most people believe that medicalizing normal childbirth is an absolute necessity, that each increased level of medicalization actually makes childbirth substantially safer and that an elective Cesarean delivery is the safest of all options, as it totally circumvents all the unpredictable dangers of normal birth.
Actual Facts: The common complications of normal childbirth in healthy women living in developed countries with functional healthcare systems are relatively rare and relatively easily and safely dealt with by modern medicine.
Artificial Dangers: However, when the same medical and surgical interventions that are so successful at treating the relatively rare (but real) complications of childbirth are routinely used on healthy women, it introduces the unnecessary risk associated with iatrogenic and nosocomial (hospital-related) complications.
As a result, highly-medicalized care in healthy women is associated with a 2- to 10-fold increase in medical interventions (EFM, immobilization in bed, induction, Pitocin-augmented labors) and Cesarean surgery (currently 33%). Unnecessary medicalization of labor and birth in healthy women is associated with increased maternal morbidity (serious complications) and elevated rate of maternal mortality in the US.
Both of easily preventable dangers are the result of the general misunderstanding of the real risks of childbirth in the 21st century.
The real elements of safety & danger as revealed by “Five Models, Five Perspectives, Five Insights:
The real source of danger for healthy childbearing women in the 21st century is lack of access to a functional health care system (Afghanistan, sub-Sahara Africa, etc) or a failure to use available maternity services, whatever the reason. This can be due to economic issues (no health insurance, trying to save money), religious or cultural beliefs, immigrations status, other personal circumstances (such as PTDS), or the result of a state-sanctioned denial-of-services by hospitals, doctors and midwives.
State-sanctioned denial of maternity care services occurs when the laws in a state allow hospitals to have policies that legally (but unethical all the same) “ban” vaginal childbirth. The result is to force unwanted Cesarean surgery on certain categories of healthy women, such as those with a ‘big’ baby, having twins, a breech baby or who previously had a Cesarean delivery. A similar legal but unethical denial-of-services occurs when malpractice carriers are allowed to lawfully prohibit obstetrical groups from providing vaginal birth services to this same subset of health women who were expecting to have a normal birth.
The last type of denial-of-services occurs when state laws for professional midwives purposefully restrict their legal ability to provide care to a subset of childbearing women. Typically this applies to essentially healthy women who have an identified risk but are decline to be medicalized against their wishes. This frequently happens to previous-CS mothers who expected to have a normal vaginal birth but finds that all the hospitals within reasonable driving distance offer only an unwanted and highly risky repeat Cesarean section.
According to constitutional law and as formally acknowledged by the American College of Obstetricians and Gynecologists (ACOG opinions #664, 214, 166 and earlier versions), adult women have a legal and ethical right to self-determination when it comes to all aspects of maternity care and childbirth services. But very often these principles are not applied to healthy childbearing women who find themselves in these situations.
When trapped between the Devil and the Deep Blue Sea by a lawful but unethical state-sanctioned denial-of-services, many of these families either seek care from lay midwives or plan an unattended birth; both decisions will unnecessarily increase easily preventable risks to mother and baby.
These are completely PREVENTABLE risks.
Part 3 (of 3)
The Silent Third Partner:
Parental Decision-Making and how the ethical and legal rights of parents to make medically unpopular or unwise choices may result in preventable neonatal mortality and how that aspect is routinely ignored in studies conducted on the relative safety of OOH birth services.
In regard to safety vs. danger in normal childbirth, we so far have focused on whether the mother-to-be had routine prenatal care vs. “no care“, an attended birth vs. unattended, whether the birth attendant was a MD or midwife, and whether the planned place-of-birth was in- or out-of-hospital.
Unacknowledged research bias on OHH Mfry Care
Of these four binary “yes/no” circumstances, two of them reflect choices made by parents — for example, to have or not have prenatal care; to have an attended vs. purposefully-unattended OOH birth — while the last two are practitioner-centric.
From the standpoint of research on OOH setting, the choice of place-of-birth is usually (though illogically) seen as a practitioner issue. The unspoken assumption is that birth attendants decide the choice of setting since each category of practitioner generally refuses to provide care to childbearing families who do not plan to give birth in the setting preferred by that birth attendant. The medical profession is firmly convinced that the whole issue of relative safety would go away in an instant if midwives would just get hospital privileges and thereafter refuse to attend home births.
That however begs the point, which is our current obstetrical-centric system as applied to healthy childbearing women. In the US, our hospital-based system steadfastly declines to provide the quality of care that families choosing OOH birth services are seeking and have an ethical right to receive — a science-based, cost-effective model specifically configured to meet the full spectrum of physical and practical needs of healthy childbearing women with normal pregnancies who do not want, need or benefit from medicalized services.
Safety research on OOH birth leaves parental decision-making out of the equation
Of the three categories of decision-makers noted above (parents, midwives & doctors), the studies on PHB/OOH only focus on the last two by only contrasting MD care vs MF care, and/or hospital vs. OOH/PHB. Regrettably, this makes relative safety into a win-loose contest: Hospital-based obstetricians versus Midwives providing care in OOH settings.
In general, midwives don’t get full credit when the outcome is good (just “lucky”), nor are they adequately credited for reducing the medical interventions 2-to-10-fold; they are however fully blamed for any possible professional inadequacy along with problems associated with an OOH environment (transfer time that delays emergency treatment).
On the other hand, the obstetrical profession is credited with all good outcomes but not held responsible for problems associated with the hospital environment and associated problems such as a high Pitocin-augmentation and C-section rate, medication mistakes, antibiotic-resistant infections and other nosocomial complications.
In both instances, parental decision-making is left out of the equation entirely, as is an equal focus on the risks and benefits of each environment — hospital as well as OOH settings. Personally, I think that is the wrong way to look at this issue, but realistically the identified ‘responsible party’ in studies on this topic is still obstetricians and midwives.
In theses instances, it’s assumed that the outcomes of midwife-attended, planned OOH births had little or nothing to do with lawful decisions make by the parents that resulted in acts or omissions that may have affected outcomes.
During prenatal care, this includes their decision to decline routine labs, pregnancy-dating and level II ultrasounds, genetic testing & termination (or refusal to terminate) a pregnancy affected by potentially lethal birth defects. During the intrapartum period, they may not tell the midwife when the water breaks before labor, or decline prophylactic antibiotic treatment when the mother is GBS+. So far as i know, only the Snowden study on PHB/OOH birth in Oregon has directly acknowledged that parental decision-making often plays a substantial role in adverse events and bad outcomes.
However, this focus on the birth attendants reduces parents to mere by-standers in someone else’s drama, and exempting them of any responsibility — good or bad — for the outcome.
In this last section, we will examine the impact of parental choice that run counter to the wishes or recommendation of their care providers or standard medical advise and in some cases, may have resulted in what appeared to be a preventable stillbirth or neonatal death.
Slient Partners: The unacknowledge role of Parental decision-making in childbirth outcomes
FACTS: The routine use of ultrasound and prenatal genetic screening in the hospital cohort, in conjunction with the termination of affected pregnancies during the pre-viable state, slightly lowers the rate of perinatal and neonatal mortality when compared to the subset of families who choose OOH birth. This is due to a reduced number of babies in the hospital cohort with lethal anomalies who are carried to term.
Families that choose non-medical maternity care are statistically less likely to utilize prenatal genetic and ultrasound screening or to terminate affected pregnancies when indicated. One study in PHB in Washington State (1996) documented a disproportionate increase NNM due to congenital anomalies, not all of which were incompatible with life. Among this specific sub-set of non-testing parents, prenatal diagnosis and planned hospital care would have reduced (but not eliminated) the incidence of neonatal mortality. However, this is a patient choice and is not a provider or place-of-birth issue.
In regard to the great debate about safety, it is useful to realize that birth-related morbidity and mortality can be time-shifted, place-shifted and practitioner-shifted, but they cannot be eliminated. In other words, increasing rates of pregnancy termination reduces neonatal mortality rates but obviously does not reduce overall perinatal mortality. There is nothing that birth attendants can do or not do that reliably, and with economically sustainability, can create a condition of zero risk for both mother and baby 100% of the time.
The risk-benefit continuum among the 4 responses to normal childbirth and the 3 types of birth attendants:
Simple access to prenatal care, on-going risk-screening and physiological management of active labor, birth and immediate postpartum-neonatal period by experienced birth attendants of all categories improved outcomes by orders of magnitude. Here is the breakdown for each type of birth attendant and both in and out-of-hospital settings.
NO CARE:
The most startling conclusion is the consequences of “no care”. Lack of prenatal care, no skilled birth attendant present during labor and birth and not having or not using emergency care when indicated is unconscionably dangerous and represents a failure of society at some level. The total absence of medical and maternity services, whether by religious or personal choice, due to poverty or cultural beliefs, can turn the otherwise normal biology of pregnancy and childbirth into a lethal condition.
LAY MIDWIVES:
Many people would have assumed that the care of lay midwives would have been little better than unattended births but they would have been very mistaken. Of the three birth attendant categories, the physiologically-based (i.e., non-medical) care by lay midwives to a demographically at-risk population demonstrated the most extraordinary level of cost-effectiveness and reduction in both maternal and perinatal mortality when compared to the control group.
When it comes to ‘value-added’ above the background biological hazard, lay midwives added the most value of any category of birth attendant. These good outcomes were achieved by providing childbearing women with prenatal care, on-going risk-screening and referring those with serious medical or pregnancy complications to obstetrical services. Mothers and their unborn babies were monitored during active labor by capable midwives who recognized medical problems and arranged timely transfer of patients with complications to the obstetrical service at the county hospital.
This straight-forward access to prenatal care, risk screening, transfer as indicated and physiological management during labor, birth and postpartum-neonatal period as provide by lay midwives was able to reduce perinatal mortality by 20 to 40 times compared to the mortality statistics for control group. This substantial feat was accomplished at a small fraction of the expense and was able to lower neonatal mortality to a rate similar to that of professional midwives and a maternal mortality rate equivalent to hospital-based-obstetrical care.
Within the structured healthcare systems of North American and the formal reimbursement scheme by governments and insurance carriers, expansion of services by lay birth attendants would not be a viable option. Our educated population rightfully expects their healthcare providers to be professionally trained, regulated by the state, able to carry emergency drugs and equipment and to repair simply perineal lacerations as a part of their normal scope of practice.
Nonetheless, lay midwives are an eager and reliable group that should not be overlooked. They are able to provide safe care within a cost-effective system that dramatically improves mother-baby safety in developing countries and among groups that are for any reason excluded from the official health care system in developed countries. It is illogical and unwise to criminalize this group.
PROFESSIONAL MIDWIVES:
In study #3 state-regulated direct-entry midwives had no maternal mortality and a neonatal mortality rate of 2.6 per 1,000 (including fatal birth defects), which was ever-so-slightly better that the lay midwives and in the same general range as hospital-based obstetrical care for low and moderate-risk women. However, childbearing women cared for by professional midwives had 2 to 10 times less obstetrical intervention than medicalized hospital care and a 6-fold decrease in Cesarean section (under 4%). All of these good outcomes were achieved at a small fraction of the expense of orthodox obstetrical care.
In study #4, the Canadian direct-entry midwives were fortunate to be providing care in a providence that had an integrated model of care with generally cooperative and complimentary relationships between midwives and physicians. Midwives in several parts of Canada have hospital admitting and practice privileges, so healthy women have the option of a planning a midwife-attended hospital birth. This also allows for continuity of care for transfers from home to hospital when the mother-to-be does not require obstetrical management or operative delivery. When the services of an obstetrician are needed, this articulated system provides for a seamless transfer of care and ‘no-fault’ receptions.
Last but not least, these statistics are for a subset of childbearing women — the lowest of low-risk women. This is a patient population with good access to and use of prenatal screening and for whom all diagnosable congenital anomalies have been eliminated from this cohort. Neonatal deaths for midwife attended PHB in this population are the very lowest of all stats for normal birth in any setting — NNM per 1,000 of 0.35 for births planned home births, 0.57 for midwife-attended hospital births, and 0.64 for physician-attended hospital births.
These are ideal circumstances and while we all aspire to them, they cannot be replicated 100% of the time by 100% of the childbearing populations. Democratic societies recognize the principle of autonomy for mentally competent adults in regard to healthcare.
With the rarest of exceptions, this general principle applies to healthy childbearing women. Assuming that the mother-to-be is fully informed by her birth attendants, she has the right to decline prophylactic medicalization and choose instead (or accept) the increase risk of a specific pregnancy or intrapartum circumstances that puts her into a moderate risk category — for example, a small fibroid, a large baby, vaginal birth after a Cesarean, prolonged rupture of membranes, meconium, or a post-dates baby with reactive NST. It is necessary for the maternity care system to acknowledge the constitutional right of adult women to continue receiving birth-related services even when they are not totally ‘ideal’ candidates for OOH care.
The alternative is to put many women between the Devil and Deep Blue Sea by denying access to professional OOH care. This forces them to choose between medicalization they do not want, and in actual fact may not benefit from, or having unattended births (the risks of which have already been identified). The other problematic possibility is that women who are refused care by regulated birth attendants will simply choose unregulated ones. This not only deprives her of access to adequately trained attendants and medical back-up arrangements but also creates another group of unregulated lay midwives, which is both unnecessary and unwise.
The better strategy is to acknowledge that moderate risk women have a constitutional right to have professional services for an OOH birth. The statistical record of a mixed-risk population (low plus moderate-risk women) consistently demonstrates a NNM rate between 1.5 and 2.6 per 1,000, irrespective of birth attendant or birth setting.
HOSPITAL-BASED CARE:
Institutionally-based obstetrical care appeared to have improved neonatal mortality ever so slightly (approximately 1.5 per 1,000) as compared to the lay attended group (3:1,000) and professional midwives (2.6:1,000, but this small gain was offset by a dramatically increasedCesarean section rate of 32% and drastically increased cost of care. This escalating CS rate has been associated with the current upward trend in maternal mortality (MM) by other researchers.
In that regard, physiologically-based forms of care, which lower the incidence of Cesarean, also reduce rates of maternal mortality. While no family or birth attendant should ever be forced to choice between the life of the baby and that of the mother, we also must be sure that enthusiasm for the lowest possible neonatal mortality statistics does not increase the risk to the childbearing woman and result in avoidable maternal mortality.
High-tech, high-cost, highly interventionist obstetrical care for healthy women does not appear to improve combined mortality rates for mothers and unborn or newborn babies. Routinely medicalizing normal childbirth in low and moderate risk mothers dramatically increases the rate of medical interventions, operative deliveries, re-hospitalization, nosocomial complications (such as MRSA infections) and 2 to 13-fold increases morbidity associated with the high rate of surgical delivery.
Bottom Line: Hospital-based obstetrical care for healthy women with normal pregnancies was not statistically safer or more cost-effective.
As measured by the outcome statistics for the 3 categories of birth attendants: lay midwife-attended, professional midwife-attended and hospital-based, medically attended — the most efficacious strategy for preventing maternal and perinatal mortality and morbidity consists of the three simple already identified aspects of maternity care that balance safety and cost-effectiveness and apply regardless of place of birth. This was associated with prenatal care, risk-screening, transfer to medical services as indicated, birth attendant skilled in physiologic care present during the intrapartum, postpartum-neonatal period and appropriate use of emergent and comprehensive medical services as necessary.
Evidence-based maternity care by birth attendants trained in physiological (non-interventive) management achieved “maximal results with minimal interventions” by a wide margin. This cost-effective care had equally good outcomes, the fewest medical and surgical procedures and least expense to the healthcare system.
To paraphrase the popular African saying, it takes a village of skilled and knowledgeable people to support the safe passage of mother and baby thru pregnancy and birth.