Part 2 (of 2)
Historical & contemporary quotes by doctors about midwives over the
last 2 centuries
on the topic of the
“the midwife problem”
The controversy within the American medical profession over what doctors historically called the “female practitioners of midwifery” began in the 18oos and simmered on the back burner for the next 200 years. It finally burst into flames in 1910 when the obstetrical profession began to hold annual meetings {Ref #1} that included sessions specifically devoted to the “midwife problem“. This referred to the problem doctors were having in their efforts to eliminate the practice of midwives in the United States.
{ref #1 ~ The American Association for the Study and Prevention of Infant Mortality -AASIM}
Needless to say, various attempts by doctors to solve the “midwife problem” been going on ever since.
Organized Medicine and “Occupational Control”
For those of you who have read Paul Starr’s exhaustive history of medical practice: “The Social Transformation of American Medicine”, will recognize this as an “occupational control” issue as defined by the AMA. This describes the ability to totally control who can practice an occupation or profession, and who can be permanently and legally locked out.
Obviously, midwives have always been on the “locked out” list!
In regard to what is legally defined as “The Healing Arts” (i.e. legislation that concerns the practice of allopathic medicine) medical lobby groups backed by the financial and political resources of the AMA, have successfully exerted total control over their “occupation” for a century or more.
This always includes legally (and often unconstitutionally) eliminating any and all forms of economic competition, no matter how trivial the issue, or how vital those now unobtainable services are to the well-being of the infants and children, childbearing women, the elderly, underserved minorities or those with untreatable chronic diseases.
 Medical lobbies typically achieve this via mammoth campaign contributions by special interest medical groups to influence legislation favorable to their group. This describes getting laws passed that make it harder, or illegal, for practitioners of a “competing” healthcare disciplines to practice.
Medical lobbies typically achieve this via mammoth campaign contributions by special interest medical groups to influence legislation favorable to their group. This describes getting laws passed that make it harder, or illegal, for practitioners of a “competing” healthcare disciplines to practice.
This also includes what is known as “regulatory capture” — getting MDs who belong to the AMA appointed to the governing boards of state regulatory agencies, such as medical, midwifery, nursing, chiropractic and naturopathic boards. This allows doctors to vote down anything that would lessen their occupational control over the practice of allopathic medicine, or reduce their economic “bottom line”.
Last but certainly not least is “yellow journalism“. Over the last century various groups of doctors, and their paid staff of lawyers and public relations expert, make deals with newspapers that they commit to spending a predetermined amount annually on advertising in their newspaper (in one documented instance that was $100,000 {Ref #2} if the paper’s editorial staff agrees to promote the agenda of organized medicine and freeze out all dissenting views and competing practitioners. This type of control over the information made available to the public is also used by pharmaceutical and health insurance companies.
{Re #2 The Social Transformation of American Medicine, 1982 and 2017, p. 265 “Committee on the Cost of Medical Care” CCMC 1926}
This amazingly upsetting and frustrating story is a long way from being over, as attested to by the number of obstetricians who seem to be obsessed with denigrating midwifery and continue to chur out anti-out-of-hospital birth studies that get published in professional journals.
In the last decade alone, this list of obstetrician-authors who regularly publish papers directly antagonists to community-based midwifery have included Amos Grunebaum, Frank Chervenak, Lawrence McCullough, J. Orosz, Birgit Arabin, JR Wax, Robert Brent, Malcolm Levene and Jenny Pang
A brief comment by the editor (that would be me!)
A Contemporary Ray of Hope
in a Still Dark Sky
I am happy to report one small ray of hope that things may getting a little better for women who choose non-medical childbirth services in their home or a free-standing birth center and the professional midwives who provide this form of community-based care.
One tiny step forward for mothers and midwives . . .
An amazing contemporary example that things may finally be moving in a positive direction is happening right now in my very own community. This week (11-30-2022) a non-profit organization called the California Maternal Quality Care Collaborative (CMQCC) hosted an online educational presentation about a very controversial and formerly taboo subject of integrating midwives and doulas into mainstream maternity care.
Personally, I never thought I’d live to see the day when the words: “midwife“, “doula” and “mainstream” were all in the same positive sentence!
But first let tell you a little bit about the CMQCC. It was founded in 2006 at Stanford University School of Medicine as a response to rising maternal mortality and morbidity rates in our state. The CMQCCis a research and educational group:
“committed to ending preventable morbidity, mortality and racial disparities in California maternity care through the use research, quality improvement toolkits, state-wide collaboratives and its innovative Maternal Data Center to improve outcomes for mothers and infants.”
Since CMQCC’s inception, California has seen maternal mortality decline by 65 percent between 2006 to 2016, while the national maternal mortality rate continued to rise!
Let me say that again, as it is so important to those families whose wife or mother did NOT die in childbirth — the coordinated activities of the CMQCC and the California Department of Health reduced maternal mortality by 65% in the last 10 years!
Why the CMQCC matters childbearing women who choose to receive care from midwives and doulas.
This bring us back to the historic and current conflict between doctors and midwives in the US. I describe this as a “Hundred Years War” waged by organized medicine against the profession of midwifery, its individual practitioners, and everything related to out-of-hospital childbirth services.
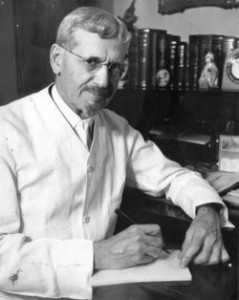
If and when the Hundred Years War were to actually end, it will be a truly historic occasion, one almost impossible for me to imagine. I was one of those midwives caught up in the “regulatory capture” of our state medical board. The majority of MDs appointed to its governing board are members of the state chapter of the AMA. Organized medicine has been fighting midwifery, and all efforts to licensed non-nurse midwives for decades, while also promoting the arrest and criminal prosecution of lay midwives.
I was one of those midwives. I was arrested in my home in Palo Alto on August of 1991 and criminally prosecuted for 20 months ($40,000 in legal expenses). The charges against me were finally dismissed in April of 1993. The unwillingness of the DA to pursue a criminal case against me, along with an editorial in the San Jose Mercury on Sunday, May 5th, 1993, finally convinced the California Medical Association (i.e. state chapter of the AMA) to stop blocking passage of the Licensed Midwifery Practice Act of 1993 (LMPA), which was signed into law October 11, 1993.
What “burying the hatchet” means to mothers and midwives
The recent presentation by the CMQCC staff also took exception to the historical prejudice by obstetricians against mothers and midwives who don’t choose, or are not affiliated with, obstetrics. The CMQCC established as a professional obligation that obstetricians and the obstetrical staff of hospitals respect the decision of childbearing women, without judgement or negative comments, who planned to give birth in a community settings.
This quality of respect also applies to the collegial relationship between the obstetrical profession and professionally-licensed community midwives. The CMQCC presentation strongly discourages the use of evocative, and often factually incorrect, vocabulary such as “failed home birth” when describing an appropriate hospital transfer, and use of “lay midwife” when the practitioner in question is state licensed and/or nationally-certified midwife.
This would also means making peace with the choice by many healthy childbearing women to have a midwife-attended birth in a non-medical setting as long as things continue to progress normally and mother and baby remain healthy. This always includes timely transfer to obstetrical services as needed.
Accepting midwives and doulas as respected members of the mainstream healthcare system would a truly historic occasion. To the surprise of many, this actually is a science-based response, as the outcomes for intrapartum care as provided by professionally-trained midwives in a non-medical setting (parents’ home or freestanding birth center) are equivalent to hospital-based obstetrics for a similar demographic of healthy childbearing women.
This is a real, but welcomed, turn-around compared to the last four decades. During most of that time, many hospital obstetrical departments in the San Francisco bay area were very vocal and even punitive in their opposed to out-of-hospital childbirth services. Whenever a hospital transfer became necessary, the conversations between attending OBs and midwives were generally very negative or they froze us out altogether.
One way this played out was for the attending OB, and sometimes the L&D nursing staff, to never look at or talk to the midwife while she was present in the room, and repeatedly refer to the intrapartum transfer as a “failed home birth”. These transfers were actually well-timed, since they preserved the welfare of mother and unborn baby. This was obvious, since no one was rushing the mother off to the OR to do an emergency C-section.
I’m sure midwives and obstetricians will always have various differences of opinion, but I can’t thank the staff of the CMQCC for such a boldly advancing the maturation of
but anyone, anywhere that reduces the maternal mortality rate is hero in my book!
So now you know about the CMQCC and can find out more by visiting their website.
Modern Maternity Care
 for Healthy Women
for Healthy Women
with Normal Pregnancies
by Faith Gibson, LM
I ~ The fundamental purpose of maternity care is to protect and preserve the health of already healthy women.
II ~ For an essentially healthy population, the safest and most cost-effective form of maternity care is always the method that provides “maximal results with minimal interventions”. This is a beneficial ratio of interventions to outcomes for each childbearing woman.
III ~ Mastery in normal childbirth services means bringing about a good outcome without introducing any unnecessary harm or unproductive expense.
IV ~ The ideal maternity care system seeks out the point of balance where the skillful use of physiological management and adroit use of necessary medical interventions provides the best outcome with the fewest number of medical and surgical procedures and least expense to the healthcare system.
V ~ Maternity care in a healthy population is ultimately judged by its results — the number of mothers and babies who graduate from its ministrations as healthy, or healthier, than when they started.
Historical & contemporary quotes
by doctors about midwives
over the last 2 centuries
on the topic of the
“the midwife problem”
I truly believe Americans will never be able to make must needed changes in the current dysfunctional obstetrical model — ones that are substantial, sustained, include an acceptance of midwifery and acknowledgment that normal birth is safer when routine interventions are NOT used.
This story has to become “common knowledge” and part of the public discourse. Can you imagine being able to understand revolutionary history without knowing about the two centuries during which America was Britain colony and we were ‘subjects’ living under the despotic rule of English kings?
They say “The Truth Shall Make you Free”. I think the truth of the obstetrical story will make doctors, midwives and mother “free”.
Prior to the 19th century, social mores considered the presence of any male, other than the mother’s husband, at a normal birth to be both indecent and improper. Since all doctors were men, this prohibition applied to them as well.
So a very curious German physician dressed himself in women’s clothing and snuck into a midwife-attended birth. Unfortunately, his rouse was quickly discovered.
Even more unfortunate for him, the family reported him to the authorities and he executed for violating contemporary morals.
1820 ~”Remarks on the Employment of Females as Practitioners in Midwifery; Published Cummings & Hilliard – Boston, 1820
….where midwifery has been in the hands of women, they have only practiced among the poorer and lower classes of people; the richer .. preferring to employ physicians, and this has been the reason why it has not become universal…
… but if it {i.e. care by midwives} is again introduced among the rich and influential, it will become fashionable; it will be considered as indelicate and vulgar to employ a physician, and the custom {i.e. the ‘female’ practice of midwifery} will become general.
It is sufficiently obvious if the employment of female practitioners becomes fashionable, that it will create a fastidious nicety of feeling, which will make it be thought indelicate to suffer the attendance of a physician…
| 5 |
1840-1847 ~ Dr Ignaz Semmelweis, physician-scientist who devoted himself to ending the pandemics of childbirth septicemia in 19th century Austria
A modern-day biography described Dr Semmelweis as:
“…one of the most prominent medical figures of his time. His discovery concerning the aetiology and prevention of puerperal fever was a brilliant example of fact-finding, meaningful statistical analysis, and keen inductive reasoning.
The highly successful prophylactic hand washings made him a pioneer in antisepsis during the pre-bacteriological era {before disposable exam gloves} and in spite of deliberate opposition and uninformed resistance {from other doctors}.”
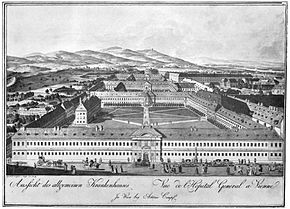
As a medical student and later as a professor of obstetrics, he worked in the lying-in wards of the world’s largest and most prestigious general hospital — the Allgemeines Krankenhaus in Vienna. In the 1840s, the maternity department housed hundreds of patients at a time, and delivered more than 3,000 babies a year. As was the custom, maternity patients stayed in the hospital for an entire month after the birth, laying around in their beds and breastfeeding their new babies (hence the concept of “lying-in wards”).
Decades before Pasteur and Lister were able to scientifically prove that bacteria caused infectious disease, Semmelweis scientifically established in 1847 that puerperal sepsis or “childbirth fever” in hospitalized maternity patient was a contagious infection spread primarily by medical students and their professors of obstetrics.
Dr. Semmelweis identified the causative factors, saying that:
…. puerperal fever is caused by the examining physician himself, by the manual introduction of cadaveric particles into bruised genitalia.
After performing autopsies on maternity patients who died the day before, med students and their professors unknowingly carried deadly germs on their hands and clothes from the hospital’s morgue to the vaginas of healthy patients in its labor wards.
In Division One, the medical school’s teaching facility for clinical training of doctors, an average of two new delivered mothers died from sepsis each day. This was a two-to-four fold increase in MMR when compared to births in the “Second Division”, which was a teaching ward run by midwives to train midwifery students. The education of midwives did not include dissecting cadavers or performing autopsies.
Having exposed the iatrogenic nature of puerperal sepsis, Dr. Semmelweis went on to develop effective methods to stop the cycle of contagion between the medical staff and their labor patients, which in turn caused more disease and more deaths. The answer started with hand washing in chlorinated lime water (i.e. bleach).
Semmelweis met with an unfortunate and early death at the age of 47 — just 21 years after starting medical school. He went more than a little crazy when he couldn’t get his professional colleagues to acknowledge the nature of this problem or use the simple measures (hand washing in chlorinated lime water) that prevented the spread of this fatal disease.
In his own words Dr. Semmelweis concluded that:
Puerperal fever is caused by conveyance to the pregnant woman of putrid particles derived from living organisms, through the agency of the examining fingers, consequently must I confession that God only knows the number of women whom I have consigned prematurely to the grave.”
~ The Allgemeines Krankenhaus ~
Poorhouse and hospital extraordinaire
Vienna’s world-famous general hospital (the Allgemeines Krankenhaus or AKH) was a huge medical complex that occupied a whole city block and at that time was the largest, most comprehensive medical facility anywhere in the world.
Like the famous Hotel Dieu in Paris, the AKH was an icon of the original concept of ‘hospital’ as a place of hospitality for the poor and homeless. Hospital care had little to do with medical cures (there weren’t any!) and everything to do with a dry bed, regular meals and someone to empty a bedpan. But soon after being founded, the AKH became part of the University of Vienna’s medical school, as its high patient census provided a bottomless pit of patients to be used as ‘teaching material’ to be used in the clinical training of medical students from all over Europe. In return for this kind of free medical care, all its patients, including women in labor, had to let themselves be used teaching cases and clinical material.
1881 ~ Transaction of the Edinburgh Obstetrical Society“, Vol. 6, Session 1880-81, Edinburgh: A discourse on childbed fever and why nurses who are menstruating are not fit to perform “certain work”
Dr. Keiller: (discussing puerperal fever) “…what he wished to insist on was that the nurses should not live in the Maternity Hospital, but someplace near. He thought that they should specially insist on nurses being very cleanly in their persons, especially during their menstruation.”
Dr. Taylor alluded to a correspondence which appeared some years ago in the British Medical Journal, affirming the truth … that a woman during her menstrual period was unfit to manipulate ham in the process of curing, the general experience being that ham so treated did not keep.
The truth was that these popular beliefs were, as a rule, the result of intelligent observation and sagacious inference, and this one at least, was supported by not only amply testimony, but constantly recurring experience.
They were all aware that whilst in some women, menstruation was a comparatively local process, in others it was accompanied by characteristic emanations from the rest of the body, and these, proceeding from the hands and reaching the pork in the process of rubbing, could hardly fail to contaminate it.
In the same manner, if these emanations be brought into contact with the raw surfaces which seem to be a necessary contingent of parturition [childbirth], how much more rapidly and certainly will mischief be done! If it affects raw pork, notwithstanding the intervention of salt used in rubbing, how much more rapidly will it be absorbed to the detriment of a living organism.
Hence there is great need for the precautions which Dr. Keiller suggests. Not only should the nurses be separately housed, but the grave question forces itself upon us, “Should a menstruating nurses be allowed to [providing care] in cases of childbirth?”
| 3 |
[**Between 1893 and 1899, the medical profession stopping using the historical word ‘midwifery’ for the medicalized management of pregnancy and childbirth and started calling it “obstetrics” instead, , this avoiding the socially awkward title of “man-midwife”.]
| 2 |
1899 ~ Dr. JW Williams’ comments on the disturbing professional rivalry between doctors who practiced obstetrics (historically a non-surgical discipline) and members of the new surgical discipline of gynecology.  General practitioners of obstetrics were not trained as surgeons, so when a labor patient needed a Cesarean section, he had to turn the case over to a gynecological surgeon.
General practitioners of obstetrics were not trained as surgeons, so when a labor patient needed a Cesarean section, he had to turn the case over to a gynecological surgeon.
This occasioned many bitter disagreements and hot tempers between the two type types of doctors, with raucous name-calling, occasional fisticuffs and mutual distrust. Dr. Williams was convinced that neither professional could advance until both joined forces to create a hybrid profession of obstetrics and gynecology as a new surgical speciality in America:
“At present, gynecology considers that obstetrics [a separate medical discipline] should include only the conduct of normal labor, or at most … cases that can be terminated without radical operative interference, while all other conditions should be brought to him [the gynecologist] — in other words, that the obstetrician should be a man-midwife.
The advanced obstetrician, on the other hand, holds that everything connected with the reproductive process of women is part of his field, and if this contention were sustained, very little would be left for the gynecologist.”
1903 ~ Quoted from Dr J. W. Williams’ famous textbook, Williams’ Obstetric, first edition, published in 1903
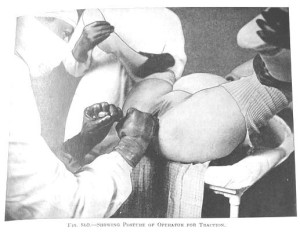
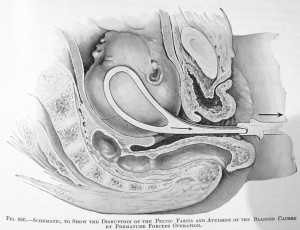
Dr. Joulin (1867) and other observers have attempted to solve the problem by calculating the force exerted in forceps deliveries. Thus, on interpolating a dynamometer between the operator and the ends of the instrument, it was found that the tractile force rarely exceeded 80, though in some cases it reached 100 pounds. A greater force than this cannot come into play, as it has been shown that .. 120 pounds is sufficient to tear the child’s head from its body.
1904 ~ The Decline in Maternal Mortality in Sweden: The Role of Community Midwifery ~ Ulf Högberg, MD, PhD August 2004, Vol 94, No. 8 | American Journal of Public Health 1312-132
The 19th century decline in maternal mortality [in Sweden] … was helped along by the national health strategy of giving midwives and doctors complementary roles in maternity care, as well as equal involvement in setting public health policy.
From 1900 through 1904, Sweden had an annual maternal mortality of 230 per 100,000 live births… For the year 1900, the United States reported 520 to 850 maternal deaths per 100,000 live births.3
The maternal mortality rate in Sweden in the early 20th century was only one third that in the United States. This rate was recognized by American visitors** as an achievement of Swedish maternity care, in which highly competent midwives attended home deliveries.
[** Several American obstetricians visited Sweden in the early 1900s to find out why their MMR was so much lower than the US]
1906 ~ Dr. Gerwin expresses his opinion about midwives:
…. the typical, old, gin-fingering, guzzling midwife, … her mouth full of snuff, her fingers full of dirt and her brain full of arrogance and superstition
1907 ~ other published comments by obstetricians about midwives:
Dr. Mabbott: … “un-American”
Drs. Emmons and Huntington: “the overconfidence of half-knowledge, …unprincipled and callous for the welfare of her patients”
1911 ~A Review of the Midwife Situation ~ Boston Medical and Surgical Journal, 02-23-1911, page 261 {*} Arthur Brewster Emmons, 2d, M.D., Boston and James Lincoln Huntington, M.D., Boston.
… we believe it to be the duty and privilege of the obstetricians of our country to safeguard the mother and child in the dangers of childbirth.
The obstetricians are the final authority to set the standard and lead the way to safety. They alone can properly educate the medical profession, the legislators and the public.”
1911 ~ Drs. Emmons & Huntington: “Has the Trained Midwife Made Good?”
The story of obstetrical education in the country is not the story of complete success. We have made ourselves the jest of scientists throughout the world by our lack of a uniform standard. TAASPIM; 1911-C, , p. 207]
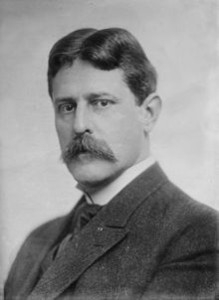
1911~ Dr J. Whitridge Williams, chief of obstetrics, Johns Hoskins, author Williams Obstetrics
| 8 |
[This] seem to indicate that women in labor are safer in the hands of …. midwives that in those of poorly trained medical men. Such conclusion however, is contrary to reason, as it would postulate the restriction of obstetrical practice to the former (midwives) and the abolition of medical practitioners, which would be a manifest absurdity.” [1911-B; p.180
1911 ~ Dr. Ira Wile, MD, New York City
In NYC, … death from puerperal sepsis occur more frequently in the practice of physicians than from the work of the midwives. [1911-G TAASPIM, p.246, 1911]
1911 ~ Josephine Baker, MD, Director, Midwifery Training program, NYC
 The irregular practitioner of medicine is still permitted to be an obstetrician with an experience that is inferior to that possessed by more than half of the midwives.
The irregular practitioner of medicine is still permitted to be an obstetrician with an experience that is inferior to that possessed by more than half of the midwives.
Let us be fair to the midwife, I say, and if she is below the ideal we have for her, though we have never crystallized that ideal into law, let us give her the opportunity to rise and educate herself … .” [1911-G; TAASPIM, p. 224]
That Socrates’ mother was a midwife bears testimony to the honorable nature of such a profession at a time when civilization in one of its highest forms was at its summit. [1911-G; TAASPIM, p. 232]
1911 ~ Dr. Ira S. Wile, MD,;New York City:
But it is manifestly unfair to criticize the lack of an educational standard which has never been established. When nurses were of the Sairey Gamp-type, elimination was not the cure. When apprenticeship was the open sesame to the practice of medicine …elimination was not the cure. Education, training, regulation and control solved these problems, just as they will solve the **midwife problem.
[**The ‘midwife problem’ usually referred to the problems some doctors were having their efforts to get rid of midwives.]
1911 ~ Dr. Emmons, MD: “Obstetrics Care in the Congested Districts of our Large American Cities”
I should like to emphasize what may be called the negative side of the midwife. Dr. Edgar states that the teaching material in New York is taxed to the utmost. The 50,000 cases delivered by midwives are not available for this purpose.
Might not this wealth of [obstetrical teaching] material, 50,000 cases in NY, be utilized to train physicians?” [TAASPIM – 1911-D, p 216]
1911 ~ A Review of the Midwife Situation; Arthur Brewster Emmons, 2d, M.D. & James Lincoln Huntington, M.D., Boston;
LEGAL SITUATION: In reviewing the midwife situation … far more might be said of the unsatisfactory condition of obstetric practice wherever the midwife exists. Two standards of skill and a divided responsibility inevitably are found.
The midwife must either be a trained obstetrician, or she must become a subordinate, co-operating with the obstetrician, as does our excellent trained obstetrical nurse, relying on his judgment and resting with him the responsibility of the two lives, before a system harmonious and satisfactory can result.
The history of temporizing with the ignorant, half-trained, often malicious midwife in our sister states to-day reads like many another misguided “freedom ” which is virtually a license by the state to practice quackery on an ignorant, unsuspecting public. The women and infants pay for this “freedom” in deaths, unnecessary invalidism and blindness.
Who are to blame? Is it the ignorant public? Shall we blame the legislators?
We believe it to be the duty and privilege of the obstetricians of our country to safeguard the mother and child in the dangers of childbirth. The obstetricians are the final authority to set the standard and lead the way to safety. They alone can properly educate the medical profession, the legislators and the public.
When such is the popular feeling, we cannot expect much result from the laws as they now exist, or in mere modification of the law. What we must first do is to arouse public sentiment, and first of all we must have the enthusiastic support and united action of the medical fraternity.
We feel that the most important change should be in the laws governing the registration of births. The word “midwife” as it occurs, should be at once erased from the statute books.
The Boston Medical and Surgical Journal, pages 251-261
1911 ~ Dr. J. Whitridge Williams, MD, Chief of Obstetrics, Johns Hopkins University Hospital
….. the ideal obstetrician is not a man-midwife, but a broad scientific man, with a surgical training, who is prepared to cope with the most serious clinical responsibilities, and at the same time is interested in extending our field of knowledge.
No longer would we hear physicians say that they cannot understand how an intelligent man can take up obstetrics, which they regard as about as serious an occupation as a terrier dog sitting before a rat hole waiting for the rat to escape. 1911-B
1911 ~ Dr. J.W Williams, MD,
The paucity of material [i.e. teaching cases] renders it probable that years may elapse before certain complications of pregnancy and labor will be observed… This is to the great detriment of the student.
Moreover, such restriction in [obstetrical] material greatly hampers the development of the professor and his assistants by the absence of suggestive problems and his inability to subject his own ideas to the test of experience. 1911-B, p. 171

1912 ~ Dr. J. Whitridge Williams:
“In Johns Hopkins Hospital,” said Dr Williams, “no patient is conscious when she is delivered of a child. She is oblivious, under the influence of chloroform or ether.
1912 ~ Dr J. Whitridge Williams:
The question in my mind is not “what shall we do with the midwife?” We are totally indifferent as to what will becomes of her…[1912-B, p.225]
No attempt should be made to establish school for midwives, since, in my opinion, they are to be endured in ever-decreasing numbers while substitutes are being created to displace them. [1912-B; p.227]
1912 ~ Dr J. Whitridge Williams continues:
Another very pertinent objection to the midwife is that she has charge of 50 percent of all the obstetrical material [teaching cases] of the country, without contributing anything to our knowledge of the subject.
As we shall point out, a large percentage of the cases are indispensable to the proper training of physicians and nurses in this important branch of medicine..” [1912-B, p.224]
In all but a few medical schools, the students deliver no cases in a hospital under supervision, receive but little even in the way of demonstrations on women in labor and are sent into out-patient departments to deliver, at most, but a half dozen cases.
When we recall that abroad the midwives are required to deliver in a hospital at least 20 cases under the most careful supervision and instruction before being allowed to practice, it is evident that the training of medical students in obstetrics in this country is a farce and a disgrace.
It is perfectly plain that the midwife cases … are necessary for the proper training of medical students.
If for no other reason, this one alone is sufficient to justify the elimination of a large number of midwives, since the standard of obstetrical teaching and practice can never be raised without giving better training to physicians.” [1912-B, p.226]
1913 ~ Dr. Van Blarcom, MD New York State:
The diagnostic ability of midwives is generally good and in the case of many, remarkable excellent. In this respect, the average midwife is fully the equal of the average physician.
1913 ~ Dr. Van Ingen and Dr. Josephine Baker, MD; for NYC
|
Birth Attendant: |
|
Midwife |
Physician |
|
Total Births (%): |
|
52% |
48% |
|
Stillbirth: |
|
10% |
90% |
|
Neonatal Deaths: |
|
35% |
65% |
1913 ~ Dr. Huntington, influential obstetrician of his day:
… the midwife will work a definite hardship to those physicians who have become well-trained in obstetrics for it will … decrease their sphere of influence.
| 8 |
1914 ~ Twilight Sleep: Simple Discoveries in Painless Childbirth
by Dr J. Whitridge Williams, MD, former professor of obstetrics, Johns Hopkins University Hospital, current Dean of the Johns Hopkins School of Medicines and Dr. H. Smith williams, MD, attorney and science writer ~ link to its 8 chapters starting with ch. 1
Dr J.W. Williams comment about the need for many thousands of “lying-in” hospitals all across America and why he considered hospitalization and Twilight Sleep to be an “incalculable boon and blessing”
“What an incalculable boon and blessing it would be, then, if conditions could be so altered that every woman brought to childbed might be insured efficient and skillful service in carrying her through the ordeal that the performance of this physiological function imposes upon her.
That word ‘physiological’ has all along stood as a barrier in the way of progress.
And this can be accomplished in no other way than has been suggested, except by the extension of a lying-in service far beyond the bounds of anything that has hitherto been attempted.
To meet their needs, it would be necessary to have a small lying-in hospital located in every town of three or four thousand inhabitants. At first thought, this seems an ideal impossible of realization. But if we consider the matter with attention, without for a moment overlooking the practicalities, we shall see, I think, that such a project by no means presents insuperable difficulties.
In time every mother in the community should come to patronize such a hospital; for it will come to be known that the home is no place for a woman during the ordeal of childbirth.
These comforts, it must be borne in mind, include the use of pain-annulling drugs. In this country, it is customary to anesthetize the patient with chloroform, though some competent practitioners prefer ether. We have already seen that the merits of the morphine-scopolamin[e] treatment, inducing the Twilight Sleep, are to be fully tested at the Johns Hopkins Hospital…
1914 ~ Dr J. Whitridge Williams, from his book “Twilight Sleep: Simple Discoveries in Painless Childbirth”
That word ‘physiological’ has all along stood as a barrier in the way of progress.
“…. the cultured woman of today has a nervous system that makes her far more susceptible to pain and to resultant shock than her more lethargic ancestor of remote generations
.… women of primitive and barbaric tribes appear to suffer comparatively little in labor, [while] civilized women of the most highly developed nervous or intellectual type who suffer most.
Even in this second decade of the 20th century, … women bring forth children in sorrow, quite after the ancient fashion, unsolaced by even single whiff of the beneficent anesthetic vapors through the use of which the agonies of tortured humanity may be stepped in the waters of forgetfulness.
 Such a woman not unnaturally shrinks from the dangers and pains incident to child-bearing; yet such cultured women are precisely the individuals who should propagate the species and thus promote the interests of the race.
Such a woman not unnaturally shrinks from the dangers and pains incident to child-bearing; yet such cultured women are precisely the individuals who should propagate the species and thus promote the interests of the race.
Abnormal pain as an evolutionary threat to the [Caucasian] race. Considered from an evolutionary standpoint, the pains of labor appear not only uncalled for, but positively menacing to the race.
…… any trait or habit may be directly detrimental to the individual and to the race and they may be preserved, generation after generation, through the fostering influence of the hot-house conditions of civilized existence.
Everyone knows that the law of natural selection through survival of the fittest, which as Darwin taught us … does not fully apply to human beings living under the artificial conditions of civilization. These artificial conditions often determine that the less fit, rather than the most fit, individuals shall have progeny and that undesirable rather than the desirable qualities shall be perpetuated.”
The problem of making child-bearing a less hazardous ordeal and a far less painful one for these nervous and sensitive women is a problem that concerns not merely the women themselves, but the coming generations.
Let the robust, phlegmatic, nerveless woman continue to have her children without seeking the solace of narcotics or the special attendance of expert obstetricians, if she prefers. But let her not stand in the way of securing such solace and safety for her more sensitive sisters.
… every patient who goes to the hospital may have full assurance that she will pass through what would otherwise be a dreaded ordeal in a state of blissful unconsciousness (i.e. Twilight Sleep drugs of scopolamine and morphine)
“In Johns Hopkins Hospital,” said Dr Williams, “no patient is conscious when she is delivered of a child. She is oblivious, under the influence of chloroform or ether.”

1914 ~ Dr. JW Williams insisted that scopolamine narcosis of women under Twilight Sleep drugs did not cause any damaging hypoxia in the fetus-neonate because neonatal respiratory depression, which delays breathing after it’s born, as actually advantageous to the newborn.
Quoted from the work of Professor Ludwig Aschoff, Dr J. Whitridge Williams explained:
“the tendency to retard respiration on the part of the child may sometimes be beneficial, preventing the infant from inhaling too early, thus minimizing the danger of strangulation from inhalation of fluids. … statistics of the Frauenklinik show that the percentage of infant mortality is low.
As against an infant mortality of 16 percent [160 baby deaths per 1,000 births] for the state of Baden, [Germany] in the same year a report on 421 ‘Twilight Sleep” babies showed a death-rate of [only] 11.6 % [ 116 per 1,000]. For this strikingly low mortality of the children during and after birth under semi-narcosis, explanation was sought of Professor Ludwig Aschoff, the great German authority on morbid anatomy.
He offered the theoretic explanation that slight narcotization of the respiratory organs during birth by extremely minute quantities of scopolamin[e] is advantageous to the child, as it tends to prevent permanent obstruction of the air-passage of children by premature respiration during birth.”
1914 ~ Twilight Sleep: Simple Discoveries in Painless Childbirth by Drs, H. Smith and J. Whitridge Williams, explaining why equal economic compensation between the sexes is not appropriate:
“Have you ever considered,” he said, “the economical significance of the fact that three out of every five women are more or less incapacitated for several days each month, and that one of them is quite unable to attend to her duties.
Granting that the two sexes are possessed of equal intelligence, it means that women cannot expect to compete successfully with men. For until they are able to work under pressure for 30 days each month, they cannot expect the same compensation as the men who do so.”
1915 ~ Dr. P.W. van Peyma, Buffalo, NY
The essential difference between a midwife and a physician is that [physicians] are free to hasten delivery by means of forceps, version, etc. This, in my experience, results in more serious consequences than any shortcomings of midwives.
Time is an element of first importance in labor, and the midwife is more inclined to give this than is the average physician. The present wave of operative interference is disastrous. … The situation would not be improved by turning [women who use midwives] into the hands of such medical men…
Obstetric training in the medical colleges is recognized as inadequate, [yet] there is no voice raised to eliminate the doctor from the practice of midwifery. Dr. Hirst is at present circularizing the State Board of Health to establish a standard for obstetrical experience for [physician] candidates for licensure, and … he suggests the personal delivery of 6 women. In NYC, the midwife is required to have the personal care of 20 women before a permit is granted to her.
1915 ~ Dr Edgar, MD, speaking about the obstetrical plan to eliminate the profession of midwifery by dividing it functions up between doctors and nurses:
Of the 3 professions—namely, the physician, the trained nurse and the midwife, there should be no attempt to perpetuate the … [midwife], as a separate profession. The midwife should never be regarded as a practitioner, since her only legitimate functions are those of a nurse …. [1915-A; p. 104]

1915 ~ Dr. Joseph DeLee, MD, obstetrician, founder of the Chicago Lying-in Hospital and Chicago Maternity Center for poor women, author of the “The Principles of Obstetrics”; identified by history as one of the two Titans and founding fathers of modern American obstetrics [Dr JW Williams being the other famous’Titian’]
Obstetrics is held in disdain by the [medical] profession and the public. The public reasons correctly. If an uneducated women of the lowest class may [provide maternity care], is instructed by doctors and licensed by the State, [attending a birth] certainly must require very little knowledge and skill — surely it cannot belong the science and art of medicine. [1915-C, p.117]
1915 ~ Dr. DeLee, “The Teaching of Obstetrics“, American Association of Obstetrics and Gynecologists
The midwife has long been a drag on the progress of the science and art of obstetrics. Her existence stunts the one and degrades the other. For many centuries she perverted obstetrics from obtaining any standing at all among the science of medicine.
The midwife is a relic of barbarism. In civilized countries the midwife is wrong, has always been wrong. The greatest bar to human progress has been compromise, and the midwife demands a compromise between right and wrong. All admit that the midwife is wrong. [TASPIM- 1915-C; .p. 114]
If the profession would realize that parturition [childbirth], viewed with modern eyes, is no longer a normal function, but that it has imposing pathologic dignity, the midwife would be impossible of mention.”[1915-C; p.117]
1917 ~ Dr. Levy, MD
These figures [refers to statistics published in 1931 by Dr. Van Ingen and Dr Josephine Baker for NYC] to certainly refute the charge of high mortality among the infants whose mothers are attended by midwives, and instead present the unexpected problem of explaining the fact that the maternal and infant mortality for the cases attended by midwives is lower than those attended by physicians and hospitals.” [1917-B; p. 44]
1921 ~ Dr. Levy examined birth-related mortality in Newark, NJ and found a similar relationship to that of Van Ingen’s survey of Manhattan (a 1913 entry above).
|
Birth Attendant: |
Midwife/Home |
Phys/Home |
Hospital |
|
Birth percentage |
38% |
30% |
31% |
|
Puerperal Deaths: |
13% |
34% |
52% |
|
Neonatal MR/1000 |
32% |
40% |
34% |
1922 ~ ELIMINATION OF THE MIDWIFE ~ Dr Ziegler, Am Assoc. for Study & Prevention of Infant Mortality ~ 1912 Transactions of its Third Annual Meeting jn Cleveland, Ohio October, 2-5, 1912 pages 222-237
Dr. Ziegler was an extremely influential obstetrician of his time and prolific writer on his favorite topic — elimination of the midwife. In this excerpt, he discusses the plan by organized medicine to drastically minimizing the time they spent providing directly care to their patients in order to maximize each doctor’s per patient profit, thereby greatly increase the physician’s income.
Dr, Ziegler and his colleagues said doctors should not waste their valuable time personally providing care during the many hours of labor, but instead should only participate indirectly as supervisors who gave instructions to the nurses who call by them if there was any question or problem.
As a result, intrapartum care during the 1st stage labor came to be defined as a nursing function provided by hospital-employed nurses who paid a very modest hourly wage. The L&D nurse’s most important duty was to call the doctor in time for him to catch the baby, thus justifying the substantial fee he would later collect from the family.
This system divided care during labor and birth between two different professions — hospital employed nurses trained to attend the laboring mother, and doctors as surgical specialists called in perform the “surgical procedure” now known as “the delivery”, in which the mother was rendered unconscious under general anesthesia, a “generous” episiotomy performed and the baby extracted by forceps.
“The doctor must be enabled to get his money from small fees received from a much larger number of patients cared for under time-saving and strength-conserving conditions;
… he must do his work at the minimum expense to himself, and he must not be asked to do any work for which he is not paid the stipulated fee.
In this plan the work of the doctors would be limited to the delivery of patients [i.e., as a surgical procedure performed by the physician], to consultant with the nurses, and to the making of complete physical and obstetrical examinations …
This means … the doctors must be relieved of all work that can be done by others —… nurses, social workers, and midwives.” [1922-A; ZieglerMD, p. 412]
“In this plan, the work of the doctors would be limited to the delivery of patients [as a surgical procedure performed by the physician], to consultants with the nurses, and to the making of complete physical and obstetrical examinations … Under this arrangements the doctors would have to work together in a cooperative association with an equitable distribution of the work and earnings.” [1922-A; ZieglerMD, p. 413]
The nurses should be trained to do all the antepartum and postpartum work, from both the doctors’ and nurses’ standpoint, with the doctors always available as consultants when things go wrong;
..midwives should be trained to act as assistant-attendants … conducting the labor during the waiting period or until the doctor arrives, and assisting him during the delivery. [1922-A, p. 413]
1923 ~ Dr. Ziegler, MD, obstetrician
As to maternal mortality, …during 1913 about 16,000 women died..; in 1918, about 23,000…and with the 15% increase estimated by [Dr.] Bolt, the number during 1921 will exceed 26,000.
1924 ~ Dr. Levy, MD
{Editor’s * I recently received an email from Dr. Levy’s grandson, who is also an MD, to tell me that when he googled his grandfather’s name, the link lead to this post and how pleased he was to hear is grandfather’s words}
….. the stationary or increasing mortality in this country associated with childbirth and the newborn is not the result of midwifery practice, and therefore their elimination will not reduce these mortality rates“, [1924-A, p. 822; Rebuttal by Dr. Levy to published remarks by Dr. Rucker, MD,]
1924 ~ The Expectant Mother ~ The Mother and Her Child’; Drs. William S. & Lena K. Sadler, M.D; section on childbirth, page 8 ~ emphasis added
“Under no circumstances should a midwife be engaged. Any reputable physician or … intellectual minister will advise that. Let your choice be either the hospital or the home; but always engage a physician, never a midwife.”
1925 ~ Dr Hardin, MD
It should be mentioned however that the US had the worst maternal-infant mortality of any country in the developed world, except for Brazil.
..in 1921 the maternal death rate for our country was higher than that of every foreign country for which we have statistics, except that of Belgium and Chile.”
… according to [Dr.] Howard maternal mortality in the [US], when compared with certain other countries, notably England, Wales and Sweden is appallingly high and probably unequaled in modern times in any civilized country.
Twenty five thousand women die in the United States every year from direct and indirect effects of pregnancy and labor
… 3 to 5% of all children die during delivery and thousands of them are crippled. [1925-A p. 347 & 350]
1926 ~ Dr. Woodbury
When the Massachusetts Supreme Court (Hanna Porn v. Commonwealth) declared midwifery to be an illegal practice of medicine in 1907, the state’s maternal mortality was 4.7 per 1000 live birth.
By 1913 it had risen to 5.6 and by 1920 it was up to 7.4
1931 ~ A report published by the White House Conference on Child Health and Protection by the Committee on Prenatal and Maternal Care, noting the wide disparity between safe care provided by midwives and the highly risky care of many physicians.
The report’s physician-authors concluded that the care of midwives was safer than the care of MDs, saying that:
“... that untrained midwives approach and trained midwives surpass the record of physicians in normal deliveries has been ascribed to several factors. (emphasis in original)
Chief among these is the fact that the circumstances of modern practice induce many physicians to employ procedures which are calculated to hasten delivery, but which sometimes result in harm to mother and child.
On her part, the midwife is not permitted to and does not employ such procedures. She waits patiently and lets nature take its course.”
|
|
|

1933 ~ Study by the New York Academy of Medicine of 2,041 maternal deaths in physician-attended childbirth*
The investigators were appalled to find that many physicians simply didn’t know what they were doing: they missed clear signs of hemorrhagic shock and other treatable conditions, violated basic antiseptic standards, tore and infected women with misapplied forceps.
|
|
At least two-thirds [of the maternal deaths], the investigators found, were preventable. … newborn deaths from birth injuries had actually increased.
Hospital care brought no advantages; mothers were better off delivering at home. … Doctors may have had the right tools, but midwives without them did better. [reported by Dr. Atul Gawande*in his 2006 New Yorker article “The Score“]
1934 ~ The Committee on Maternal Welfare of the Philadelphia County Medical Society
…. expressed concern over the rate of deaths of infants from birth injuries increased 62% from 1920 to 1929. This was simultaneous with the decline of midwife-attended birth and the increase in routine obstetrical interventions, due in part to the influence of operative deliveries.
Excerpt, Dr. Neal DeVitt, MD, a 1975 doctoral thesis: “The Elimination of Midwifery in the United States — 1900 through 1935
1937 ~ obstetrician and famous philanthropist Dr. Alan Guttmacher (associate professor of obstetrics, John Hopkins Hospital) from his book “Into This Universe”:
Though we cannot make an exact comparison between the maternal mortality in the United States and that in European countries, we can at least make a rough comparison.
All who have studied the problem agree that the rate [of good outcomes] for Holland, Norway, Sweden, Denmark is far superior to our own. Why? … it must be due to … the patients themselves and differences in the way that pregnancy and labor are conducted in the two regions.
What about the conduct of labor in the two regions? Here is where the major differences lie. In the first place, … at least 10 percent of labors in this country are terminated by operation. In the New York Report 20 percent of the deliveries were operative, with a death rate of more that 1 in each 100 of the operated, and 1 in 500 of those who delivered spontaneously.
| Very depressed baby, likely from narcotics during labor & general anesthesia during birth Note –> umbilical cord is empty of blood and not pulsing @ the time of the birth |
 |
Let us compare the operative rates of these relatively dangerous countries (USA, Scotland) with those of the countries which are safer. In Sweden the [operative] interference rate is 3.2 percent, in Denmark it is 4.5, while in Holland ….. it is under 1 percent.
What is responsible for this vast difference in operative rates? … Analgesics [narcotic drugs] and anesthetics, which unquestionably retard labor and increase the necessity for operative interference, are almost never used by them in normal cases; and more than 90 percent of their deliveries are done by midwives unassisted.
And midwives are trained to look upon birth as a natural functions which rarely requires artificial aid from steel or brawn. [1937-A,p. 133-134]
1937 ~ Dr. Allan Guttmacher, quoting a 1932 speech by Dr. Louis Dublin, President of the American Public Health Association, and statistician for the Metropolitan Life Insurance Company, on maternal-infant outcomes by the Frontier Nurses’ midwifery service in rural Kentucky during the previous two years:
We have had a … convincing demonstration by the Frontier Nursing Service of Kentucky of what the well-trained midwife can do in America. …. The midwives travel from case to case on horseback through the isolated mountainous regions of the State. There is a hospital at a central point, with a well-trained obstetrician in charge, and the very complicated cases are transferred to it for delivery.
..they have delivered over 1,000 women with only two deaths — one from heart disease, the other from kidney disease. During 1931 there were 400 deliveries with no deaths. The study shows conclusively that the type of service rendered by the Frontier Nurses safeguards the life of the mother and babe.
If such service were available to the women of the country generally, there would be a savings of 10,000 mothers’ lives a year in the US, there would be 30,000 less stillbirths and 30,000 more children alive at the end of the first month of life [70,000 preventable maternal-infants deaths a year]. ***
 |
 |
 |
 |
What are the advantages of such a system? It makes it economically possible for each woman to obtain expert delivery care, because expert midwife is less expensive than an expert obstetrician. Midwives have small practices and time to wait; they are expected to wait; this is what they are paid for and there they are in no hurry to terminate labor by ill-advised operative haste.” [1937-A]
1966 ~ Dr. J. Rovinsky, MD; foreword of Davis Obstetrics:
“There is no alibi for not knowing what is known“
1971 ~ Dr. Levy, et al ~ Published report on a California nurse-midwife pilot program at Madera County Hospital from July 1960 to June 1963 that served mainly poor agricultural workers.
During the three-year program, prenatal care increased and prematurity and neonatal mortality rate decreased at the county hospital.
After it was discontinued by the California Medical Association, the neonatal mortality rate increased even among those women who had received no prenatal care.
This suggests that the intrapartum care delivered by nurse-midwifes may have been far more skillful than that delivered by physicians. Prenatal care decreased while prematurity rose from 6.6 to 9.8% and neonatal mortality rose from 10.3 to 32.1 per 1,000 live births.
It was concluded that the discontinuation of the nurse-midwives’ services was the major factor in these changes.
1975 ~ New York Times Magazine
In the United States … in the early part of this century, the medical establishment forced midwives — who were then largely old-fashioned untrained “grannies” — out of the childbirth business. Maternal and infant mortality was appallingly high in those days…
As the developing specialty of obstetrics attached the problem, women were persuaded to have their babies in hospitals, and to be delivered by physicians …. Today it is rare for a women to die in childbirth and infant mortality is (low) …“ [Steinmann, 1975]
1977 ~ Letter from Dr. Heinrichs, MD., Ph.D., August 1, 1977, Stanford University Medical Center to the State Legislature, strongly opposing AB 1896, the first of 6 failed direct-entry (non-nurse) midwifery licensing bill:
If we want an increase in cerebral palsy, mental retardation, extended hospitalizations for mothers undergoing infections, fistulas, hemorrhages, and other severe and disabling results of neglected childbirth, only then could one endorse bill AB 1896.
1985 ~ Drs. Feldman and Friedman: “Prophylactic Cesarean Section at Term?”
This peer-reviewed paper in the NEJM proposed that the prophylactic use of Cesarean section become new standard of care for all childbearing women, claiming that pre-labor Cesarean surgery would ‘save’ 36 to 360 babies for every one “extra” woman dying from complications of their elective surgical delivery.
p. 1266 ….the number of extra women dying as a result of a complete shift to prophylactic cesarean section at term would be 5.3 per 100,000….
This may be the proper moment to recall that the number of fetuses expected to suffer a disaster after reaching lung maturity is between 1 in 50 to 1 in 500. … if it could save even a fraction of the babies at risk, these calculations would seem to raise the possibility that a shift toward prophylactic cesarean section at term might save a substantial number of potentially healthy infants at a relatively low cost of excess maternal mortality.
We probably would not vary our procedures if the cost of saving the baby’s life were the loss of the mother’s. But what if it were a question of 2 babies saved per mother lost, or 5 or 10 or (as our calculations roughly suggest) as many as 36 or 360? …. Is there some ratio of fetal gain to maternal loss that would unequivocally justify a wider application of this procedure?
p. 1267….is it tenable for us to continue to fail to inform patients explicitly of the very real risks associated with the passive anticipation of vaginal delivery after fetal lung maturity has been reached?
If a patient considers the procedure and decides against it, must she then be required to sign a consent form for the attempted vaginal delivery?
“Prophylactic Cesarean Section at Term?”; Feldman GB, Friedman JA;
New England Journal of Medicine 1985;312:1264-1276
1992 ~ A refreshingly honest comment by Dr. JA Macer, MD, published in an obstetrical journal, admitting that:
It is no longer feasible for individual physicians who have invested 12 years in training at a cost of hundreds of thousands of dollars to dedicate extended periods to observing one normal woman in labor. [Macer JA et al; Am J Obstet Gynecol 1992:166:1690-7].
1996 ~ A report on the rising cesarean delivery published by the Medical Leadership Council (an association of more than 2,000 US hospitals), concluding that:
“the US cesarean rate was medicine’s equivalent of the federal budget deficit; long recognized as [an] abstract national problem, yet beyond any individual’s power, purview or interest to correct.”
1997 ~ email comment from an obstetrician
In my opinion issuing a license to a [non-nurse or direct-entry] midwife is giving away a license to kill. … I think licensing this activity in the name of competition is wrong. In the name of quality of care it’s wrong. In fact, it’s just plain wrong” [email correspondence 08:38am 1/17/97 from dk:ob-gyn-l@obgyn.net]
1998 ~ Betsy Hyde, CMN, hospital practice privileges & Assistant Clinical Professor, Yale University ~ posted on a popular ObGyn ListServ in response to negative comments by obstetricians about the practice of midwifery
Please, let us not take this into a “them vs. us” flame war. That benefits neither of us, our clients, the list or life in general. My original post was simply to state that midwives are safe, appropriate practitioners, and we have good outcome data to support our practice. I posted an article from the Journal of Epidemiology and Public Health to reiterate the safety of midwifery care. IMO collaborative practice with obstetricians and midwives is the most appropriate practice
Reply by Dr Suleman, MD
This was exactly my point – a crap article in a crap journal and the midwives have fooled the HMOs, the women’s magazines, Oprah and almost fooled all the OBs on the List. … If the OBs want to protect their ground in the , you better start fighting all nonsense opposition as strongly as possible. The HMOs are killing you guys because you guys were too busy making money and were not interested in the politics of medicine. Aristotle said: “If you don’t get involved in politics, be prepared to be ruled by a person lesser than you.
1998 ~ Professor Mahmoud F. Fathalla, Professor of Obstetrics and Gynaecology & former Dean of the Medical School at Assiut University, Egypt; Chair of the WHO Advisory Committee on Health Research.
The question should not be: ‘why do women not accept the service we offer‘, but
‘why do we not offer a service that women will accept?’
2006 ~ Drs De Vries & Lemmens
While looking for a scientific explanation for the extremely high use of obstetrical interventions during labor and birth in healthy women with normal pregnancies, the authors noticed that obstetrical research tended to follow the popular trends in practice, rather than lead.
This turns the idea the scientific method of inquiry on its head, as ‘evidence-based decision making‘ is displaced by ‘decision-based evidence-making‘:
… an expectant and patient approach to birth…, where all is considered normal until proved otherwise, produces a science that proves {routine} intervention to be unnecessary.
Alternatively, an aggressive approach to birth…, where birth is regarded as normal only in retrospect, generates a science that demonstrates the need for monitoring and intervention
…. evidence suggests that mainstream obstetric science follows mainstream obstetric practice. (p. 2704).
** De Vries R, Lemmens T. The social and cultural shaping of medical evidence: case studies from pharmaceutical research and obstetric science. Soc Sci Med 2006;62(11):2694-706.
2011 ~ Rachael Ward, director of research for Amnesty International USA and author of: “Deadly Delivery: The Maternal Health Care Crisis in the USA.
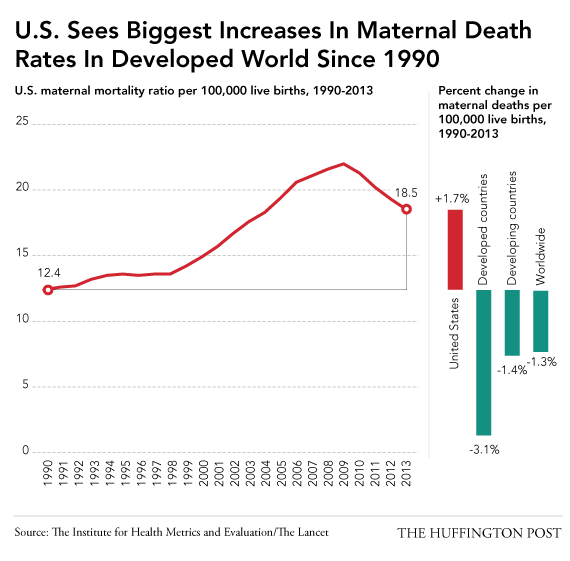
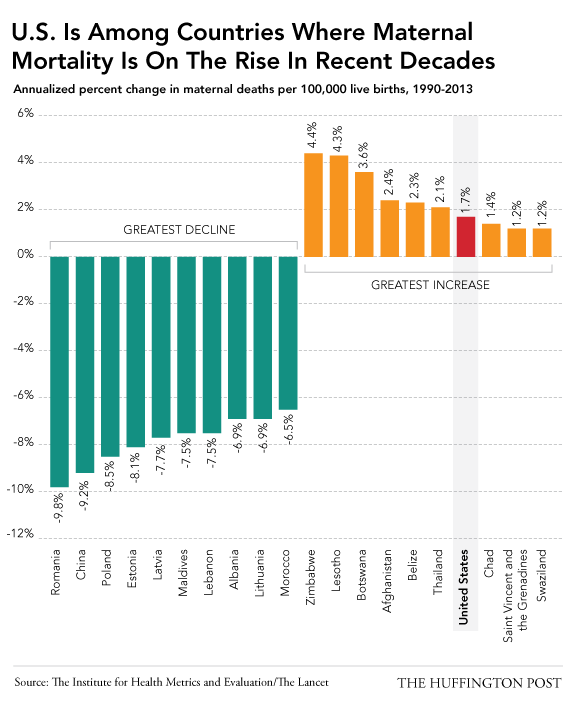
When Rachel Ward of Amnesty-USA was interviewed about maternal mortality rates (MMR), she applauded the decline in maternal mortality rates worldwide, but noted that the the United States was one the exceptions.
“eight countries are bucking that trend, with the U.S. as the only developed nation among them.
.We’re not waiting for a medical breakthrough, what we’re waiting for here is the political will”
She went on to describe maternity care issues in the US as complex, systemic and basically political, and includes the financial interests of the dominant system, and ability of special-interest lobbying groups to endlessly perpetuate the status quo, irrespective of scientific evidence or common-sense.
2014 ~ Excerpts from an On-line news story about rising maternal mortality rate in the US and work by the Institute for Health Metrics and Evaluation, a global health research center at the University of Washington.
After the Institute gathered 20 years of worldwide maternal health data, their research team identified 18.5 maternal deaths per 100,000 live births in the U.S., up from 12.4 deaths per 100,000 births in 1990.
Their most recent report, which was later published in the Lancet, American maternal mortality rates over that 20-year period rose at a rate that puts the U.S. in the company of war-torn countries like Afghanistan and impoverished nations like Chad and Swaziland. When Dr. Nicholas Kassebaum, lead author of the study and a Seattle Washington pediatrician, was interviews he stated that
“the US ranks 60th in the world, which is below virtually every other developed nation. … We’re close to triple the (MM) rate of the U.K., and eight times higher than Iceland, the world’s leader”.
2016 ~ The Final Solution to the Midwife Problem:
From the perspective of the American obstetrical profession, the ‘midwife problem’ was solved to their satisfaction between 1910 and 1940 by legally eliminating the traditionally independent practice of midwifery in the United States.