1 Guidelines relative to AB 1308
2. Two other helpful and politically interesting Links (very interesting!)
3. Midwifery Defined & comparing historical birth images and artwork
4. Current version of practice guidelines as informally adopted by the MBC as non-binding (not legally enforceable), as of May 2014
@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@
(1) Standard or Care for Ca LMs as adopted by the MBC in 2006 AND what are now called “Practice Guidelines” that reflect the changes, deletions, & additions required by Ab1308 and the fact that as mere guidelines, they do not provide the same high level of legal practice that applies to an actual “Standard” of care.
 MBC_2014-Compare-2006-SofC_vs_ClinGdelines_Oct-9-2014
MBC_2014-Compare-2006-SofC_vs_ClinGdelines_Oct-9-2014
This link opens a comparison PDF that compares both pre- and post-AB 1308 in the same document. This uses the same format as pending legislation & regulations (see key below).
Of particular interest is page 9, which has our original standard of care definition of the LMs responsibility to inform and recommend medical evaluation and the client’s Rights of Self-determination and other safeguards against involuntary medicalization OR denial of prenatal and intrapartum services
KEY to text is in PDF is as follows:
BLACK = no change
Red text = added by MBC
Blue text = ethical concepts accepted by MBC that help us and provide some protection to CB families
STRIKE-THRU’s = Are DELETED text by the MBC that eliminate patient rights & forces involuntary medicalization
@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@@

(2) Other helpful and politically interesting Links
(a) Final Version: Social and Political History of California ~ 1850 to 2014
(b) Historical and Contemporary comments by physicians about midwives ~ 1820 to 2014
@@@@@@@@@@@@@@@@@@@@@@@@@@@@
(3) Midwifery Defined ~ also comparing historical birth images and artwork.
The set begins with unencumbered women in 2nd stage labor in various supported upright positions with the “midwife/obstetric” standing or crouching in front of the mother to received the baby and hand it up to the mother, or in some cases, lying back on a divan, bed or deep water pool and pushing the baby out into the midwife’s waiting hands and she hands the new baby up to its new mother.
 |
 |
 |
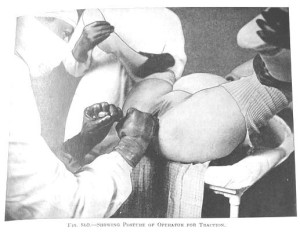
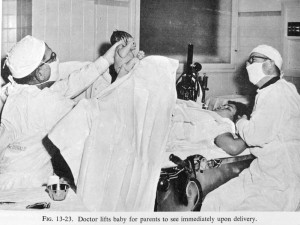
Over the last few centuries, this transitioned to an increasingly encumbered and bedded woman giving birth on her back like a stranded beetle. Beginning in 1910, the laboring woman narcotics during labor, such as the use of Twilight Sleep drugs. After being moved by stretcher from the labor ward to the OR-type delivery room, her hands would be put in leather wrist restraints, lest she accidentally touches something and contaminates the doctor’s sterile field. Her legs would be strapped into stirrups, her crotch scrubbed with an antiseptic soap, and her body covered up under mounds of serial sheets.
When the doctor arrived, the mother-to-be was rendered unconscious under general anesthesia. The physician-obstetrician then deftly performed a ‘baby-ectomy’ using ‘low’ forceps. In these circumstances, women no longer gave birth — doctors ‘performed’ the surgical procedure of vaginal ‘delivery’ while the mother was unconscious.
|
|
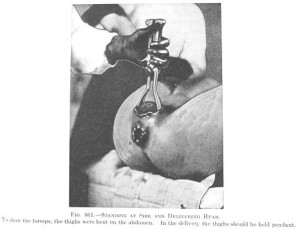
In many (but not all) parts of the county, spinal and pudendal blocks (a form of local anesthesia), and eventually epidurals during labor and birth replaced general anesthesia by the 1960, the 70s and 80s. Women were no longer unconscious (although the labor patient in the picture looks like so be happier if she were), but labor and birth were still heavily medicalized and women moved to the delivery room for the birth.
 |
 |
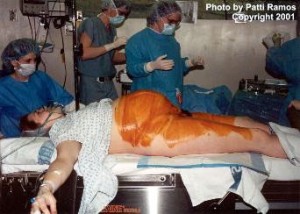
By the 1900s and early 2000s, upgraded obstetrical had replaced the routine use of the delivery room with LDRP beds that can be taken apart and turned into a gynecology-type OR table. Also the mandatory use of OR-garp had been relaxed and surgical masks were no longer mandatory. However women under epidural are still unable get out of bed or move about very well, so they also lay on their backs, still pushed the babies out over empty space to be ‘caught’ by the masked stranger standing at the end of the LDRP delivery table.
For women who were not anesthetized, the head of their bed was sometimes gatched up so they were no longer flat on their back when the (now) unmasked stranger caught their baby.
A few lucky women managed to use a squatting bar, or “allowed” to give birth lying on their side. This was an improvement but note — the labor woman’s feet still never get to touch the ground, she is never allowed to be a physically free agent, so that she can hold up her own body, and move about as she needs or wants to.
This very depressing story culminates in the late 20th and early 21st century with the laboring woman strapped to an OR table in the classic “crucifix” position and the masked and hooded OR staff pulling her baby out of a Cesarean surgery incision.
@@@@@@@@@@@@@@@@@@@@@@@@@@@
 Final Version ~ Social & Political History of California Midwifery ~ 1850 to 2014
Final Version ~ Social & Political History of California Midwifery ~ 1850 to 2014
Teaser Read:
Midwifery is the first organized healthcare discipline, with historical roots that trace back 5,000 years to ancient Egypt.
A healthcare discipline is one that protects, promotes and preserves health. Maternity care in particular is concerned with preserving, protecting and promoting the health of already healthy childbearing women. Historically midwives have provided maternity care as a supportive and non-medical process. {continue reading by clicking above link}
@@@ May 2104 @@@
Current version informally adopted by the MBC as non-binding (not legally enforceable) “guidelines”
MEDICAL BOARD OF CALIFORNIA
PRACTICE GUIDELINES
FOR CALIFORNIA LICENSED MIDWIVES
May 2014
The California licensed midwife is a professional health care practitioner who offers primary care to healthy women and their normal unborn and newborn babies throughout normal pregnancy, labor, birth, postpartum, the neonatal and inter-conceptional periods.
I. PURPOSE, DEFINITIONS & GENERAL PROVISIONS
A. This document provides a framework to identify the professional responsibilities of licensed midwives and permit an individual midwife’s practice to be rationally evaluated, to ensure that it is safe, ethical and consistent with the professional practice of licensed midwifery in California. However, these practice guidelines are not intended to replace the clinical judgment of the licensed midwife.
Sources and documentation used to define and judge professional practice include but are not limited to the following:
- The international definition of a midwife and the midwifery scope of practice
- Customary definitions of the midwifery model of care by state and national midwifery organizations, including the Licensed Midwifery Practice Act of 1993 and all it amendments (Business and Professions Code Sections 2505, et seq.)
- Standards of practice for community midwives as published by state and national midwifery organizations
- Philosophy of care, code of ethics, and informed consent policies as published by state and national midwifery organizations
- Educational competencies published by state and national direct-entry midwifery organizations
B. The California licensed midwife maintains all requirements of state and, where applicable, national certification while keeping current with evidence-based and ethical midwifery practice in accordance with:
- The body of professional knowledge, clinical skills, and clinical judgments described in the Midwives Alliance of North America (MANA) Core Competencies for Basic Midwifery Practice
- The statutory requirements as set forth in the Licensed Midwifery Practice
Act of 1993 (“LMPA”), all amendments to LMPA and the Health and SafetyPage 1 Code on birth registration. - The generally accepted guidelines for community-based midwifery practice as published by state and national direct-entry midwifery organizations
C. The California licensed midwife provides care in private offices, physician offices, clinics, client homes, maternity homes, birth centers and hospitals. The licensed midwife provides well-women health services and maternity care to essentially healthy women who are experiencing a normal pregnancy. An essentially healthy woman is without serious pre-existing medical or mental conditions affecting major body organs, biological systems or competent mental function. An essentially normal pregnancy is without serious medical complications affecting either mother or fetus, and is consistent with the definition set forth under Business and Professions Code Section 2507 (b)(1).
- The California licensed midwife provides the necessary supervision, care and advice to women prior to and during pregnancy, labor and the postpartum period, and conducts deliveries and cares for the newborn infant during the postnatal period. This includes preventative measures, protocols for variations and deviations from norm, detection of complications in the mother and child, the procurement of medical assistance when necessary and the execution of emergency measures in the absence of medical help.
- The California licensed midwife’s fundamental accountability is to the women in her care. This includes a responsibility to uphold professional standards and avoid compromise based on personal or institutional expediency.
- The California licensed midwife is also accountable to peers, the regulatory body and to the public for safe, competent, ethical practice. It is the responsibility of the licensed midwife to incorporate ongoing evaluation of her/his practice, including formal or informal sources of community input. This includes but is not limited to the licensed midwife’s participation in the peer review process and any required mortality and morbidity reporting. The results of these individual evaluations can be distributed to influence professional policy development, education, and practice.
- The California licensed midwife is responsible to the client, the community and the midwifery profession for evidence-based practice. This includes but is not limited to continuing education and on-going evaluation and application of new information and improved practices as recommended in the scientific literature. It may also include developing and dispersing midwifery knowledge and participating in research regarding midwifery outcomes.
H. The California licensed midwife uses evidence-based policies and practice guidelines for the management of routine care and unusual circumstances by establishing, reviewing, updating, and adhering to individualized practice policies, guidelines and protocols appropriate to the specific setting for a client’s labor and birth and geographical characteristics of the licensed midwife’s practice. Practice-specific guidelines and protocols are customarily implemented through standard or customized chart forms, informed consent and informed refusal documents (including the consent required in Business and Professions Code Section 2508), other formal and informal documents used routinely for each area of clinical practice, including but not limited to the antepartum, intrapartum, postpartum, newborn periods and inter-conceptional periods..
I.?
J.?
The licensed midwife’s policies, guidelines and protocols are consistent with standard midwifery management as described in standard midwifery textbooks or a combination of standard textbooks and references, including research published in peer-review journals. Any textbook or reference which is also an approved textbook or reference for a midwifery educational program or school is considered an acceptable textbook or reference for use in developing a midwife’s individual policies and practice guidelines. When appropriate or requested, citations of scientific sources should be made available for client review.
The licensed midwife may expand her skill level beyond the core competencies of her training program by incorporating new procedures into the individual midwife’s practice that improve care for women and their families. It is the responsibility of the licensed midwife to:
1. Identify the need for a new procedure by taking into consideration consumer demand, standards for safe practice, and availability of other qualified personnel.
2. Ensure that there are no institutional, state, or federal statutes or regulations that would constrain the midwife from incorporating the procedure into her practice.
3. Be able to demonstrate knowledge and competency, including:
a) Knowledge of risks, benefits, and client selection criteria.
b) Having a process for acquisition of required skill for identifying and managing complications.
d) Employing a process to evaluate outcomes and maintain professional competency.
4. Identify a mechanism for obtaining medical consultation, collaboration, and referral related to each new procedure.
II. A BRIEF OVERVIEW OF THE LICENSED MIDWIFE’S DUTIES AND SPECIFIC RESPONSIBILITIES TO CHILDBEARING WOMEN AND THEIR UNBORN AND NEWBORN BABIES
A. The California licensed midwife engages in an ongoing process of risk assessment that begins with the initial consultation and continues throughout the provision of care. This includes continuously assessing for normalcy and, if necessary, initiating appropriate interventions including consultation, referral, transfer, first-responder emergency care and/or emergency transport.
B. Within the midwifery model of care, the licensed midwife’s duties to women and babies include the following individualized forms of maternity care:
- Antepartum care and education, preparation for childbirth, breastfeeding and parenthood.
- Risk assessment, risk prevention and risk reduction.
- Identifying and assessing variations and deviations from normal and detection of abnormal conditions and subsequently communicating that information to the woman and, when appropriate, to other healthcare providers and emergency responders.
- Maintaining an individual plan for consultation, referral, transfer of care and emergencies.
- Evidence-based physiological management to facilitate spontaneous progress in labor and normal vaginal birth while minimizing the need for medical interventions.
- Procurement of medical assistance when indicated.
- Execution of appropriate emergency measures in the absence of medical help.
- Postpartum care to mother and baby, including counseling and education.
- Maintaining up-to-date knowledge in evidence-based practice and proficiency in life-saving measures by regular review and practice.
- Maintenance of all necessary equipment and supplies, and preparation of documents including educational handouts, charts, informed consent & informed refusal documents (including the consent required in Business and Professions Code Section 2508), birth registration forms, newborn screening, practice policies, guidelines, protocols, and, morbidity and mortality reports and annual statistics.
III. GUIDELINES FOR COMMUNITY-BASED MIDWIFERY
ONE: The licensed midwife is accountable to the client, the midwifery profession and the public for safe, competent, and ethical care.
TWO: The licensed midwife ensures that no act or omission places the client at unnecessary risk.
THREE: The licensed midwife, within realistic limits, provides continuity of care to the client throughout the childbearing experience according to the midwifery model of care.
FOUR: The licensed midwife respects the autonomy of the mentally competent adult woman by working in partnership with her and recognizing individual and shared responsibilities. The midwife recognizes the healthy woman as the primary decision maker throughout the childbearing experience.
FIVE: The licensed midwife upholds the client’s right to make informed choices about the manner and circumstance of pregnancy, and childbirth, and facilitates this process by providing complete, relevant, objective information in a non- authoritarian and supportive manner, while continually assessing safety considerations and risks to the client, informing her of same.
SIX: The licensed midwife refers the client to a physician, as required by law, if at any point during a pregnancy, childbirth, or postpartum care the client’s condition deviates from normal.
SEVEN: The licensed midwife confers and collaborates with other healthcare professionals, including other midwives, as is necessary to professionally meet the client’s needs. When the client’s condition or needs exceed the midwife’s scope of practice or personal practice guidelines, the licensed midwife consults with and refers or transfers the client to a physician or other appropriate health care provider.
EIGHT: Should the pregnancy deviate from normal and primary care be transferred to a physician, the licensed midwife may continue to counsel, support and advise the client at her request.
NINE: The licensed midwife maintains complete and accurate healthcare records.
TEN: The licensed midwife ensures confidentiality of information except with the client’s consent, or as required to be disclosed by law, or in extraordinary circumstances where the failure to disclose will result in immediate and grave harm to the client, baby or other immediate family members or professional care providers.
ELEVEN: Where geographically feasible, the licensed midwife makes a good faith effort to ensure that a second midwife, or a qualified birth attendant certified in neonatal resuscitation and cardiopulmonary resuscitation, is available during the delivery.
TWELVE: The licensed midwife orders, uses or administers only those drugs, supplies, devices and procedures that are consistent with the licensed midwife’s professional training as described in 16 CCR 1379.30, community standards and the provisions of LMPA and does so only in accordance with the client’s informed consent.
THIRTEEN: The licensed midwife orders, performs, collects samples for, or interprets those screening and diagnostic tests for a woman or newborn which are consistent with the licensed midwife’s professional training, community standards, and provisions of the LMPA, and does so only in accordance with the client’s informed consent.
FOURTEEN: The licensed midwife participates in the continuing education and evaluation of self, colleagues and the maternity care system.
FIFTEEN: The licensed midwife critically assesses evidence-based research findings for use in practice and supports research activities.